|
|
 |
 |
 |
 |
|
|
Orbit/Oculoplastics Quiz 14
|
Printer Friendly
|
|
|
|
[Back to Questions] [Back to Orbit/Oculoplastics]
|
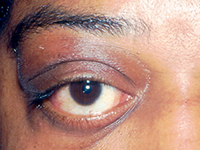
Figure 1.
|
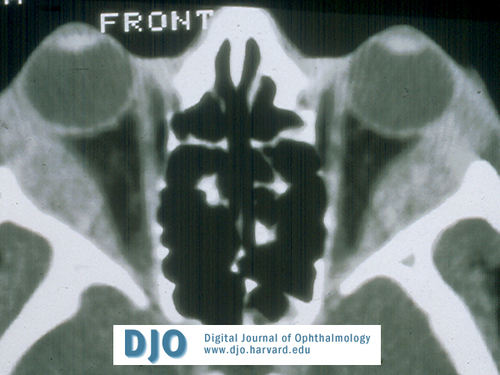
Figure 2.
|
| | Case History | | This 50 year old African American woman presented with a 6 month history of painless, progressive bilateral lacrimal enlargement without any other ocular complaints. | | | Questions and Answers | 1. What is the differential diagnosis for chronic, bilateral lacrimal gland enlargement?
Answer: The causes of chronic bilateral dacryoadenitis are generally systemic disorders, which can be grouped into 3 main categories:
Infectious:
Most commonly viral, including EBV, mumps (particularly in children), CMV, HZV, echovirus, and coxsackie virus A.
Bacterial dacryoadenitis is generally acute in onset, but atypical organisms such as syphilis and tuberculosis commonly present with a relatively indolent course.
Autoimmune:
Idiopathic inflammatory pseudotumor
Sarcoidosis
Sjogren’s syndrome
Lymphoproliferative disease:
Lymphoid hyperplasia
Lymphoma
Multiple myeloma
Leukemia
2. What other information from the patient’s history and examination would be helpful in narrowing the diagnosis?
Answer: Ocular pain, particularly pain that is exacerbated by eye movement or accompanied by diplopia, is almost always associated with idiopathic orbital pseudotumor. Pain may or may not be present with infectious causes, sarcoidosis, or Sjogren’s syndrome. In contrast, lacrimal gland enlargement caused by the lymphoproliferative disorders is almost always painless and rarely causes diplopia or limitation of eye movement. Photophobia and blurred vision would suggest additional uveal inflammation which is characteristic of sarcoid whereas dry eye symptoms might indicate Sjogren’s syndrome.
Other clues from the review of systems could include constitutional complaints such as fever, malaise, fatigue, weight loss or other indicators of systemic autoimmune disease, malignancy or infection. Viral infection might be more likely in previously healthy individuals with a flulike prodrome, respiratory symptoms, and little less on review of systems. Shortness of breath or persistent cough, and/or skin rash would be suggestive of sarcoidosis while xerostomia, dryness of other mucous membranes and parotid gland enlargement are associated with Sjogren’s syndrome. Additionally, since other systemic autoimmune disorders such as systemic lupus erythematosis, rheumatoid arthritis, scleroderma and mixed connective tissue disease are correlated with Sjogren’s, symptoms such as malar or discoid skin rash, changes in skin consistency, oral/nasal ulcers, and arthritis might also be helpful.
On examination, a tender lacrimal gland with swelling of the adjacent lateral upper lid and local conjunctival injection could point to infection or orbital pseudotumor. The presence of keratic precipitates (“mutton fat”), iris nodules, anterior vitreous cell (“snowballs”), posterior synechiae with or without an associated increase in IOP secondary to angle closure, cystoid macular edema, retinal perivenular granulomas (“candlewax drippings”) or perivascular sheathing, or increased IOP would be consistent with sarcoid uveitis. Decreased tear production of Schirmer’s testing with or without associated epithelial keratopathy suggest Sjogren’s while preauricular or mandibular lymphadenopathy might suggest either infection or malignancy.
3. What additional tests would help to confirm the diagnosis?
Answer: Depending on the clinical history, initial general laboratory tests may include CBC with differential, viral antibody titers, ESR, ANA, ACE, RPR, FTA. More specific assays for autoimmune antibody titers (e.g. anti-Ro and anti-La, CH50, C3, C4, RF) would be indicated if there is high suspicion for a particular autoimmune disease, and bone marrow biopsy might be considered for a likely malignancy.
With regard to imaging, in the setting of bilateral dacryoadenitis, orbital CT is useful in delineating the size and extent of the lesions and the involvement of other orbital structures. In the case of chronic infectious dacryoadenitis, there may be rim enhancement which is not characteristic of other causes. Orbital pseudotumor may demonstrate posterior or circumferential scleral thickening, or extraocular muscle enlargement. In general, however, CT alone is not practical in differentiating the possible diagnoses which all tend to demonstrate enlarged, enhancing lacrimal glands with or without local fat stranding. Chest XR or CT can help to diagnose pulmonary sarcoid (i.e. hilar lymphadenopathy) or rarely, tuberculosis. When the clinical findings are inconclusive and there is suspicion for an inflammatory or malignant etiology, biopsy is indicated.
4. How would you manage this patient?
Answer: Transconjunctival biopsy of the lacrimal gland from this patient showed the presence of epithelioid cells and noncaseating granulomatous inflammation that is characteristic of sarcoidosis. Additionally, ACE levels were elevated and CXR demonstrated bilateral, perihilar lymphadenopathy.
For anterior uveitis, cycloplegia is necessary for comfort and to prevent formation of posterior synechiae and associated secondary glaucoma. Topical steroids are titrated to the degree of anterior chamber inflammation. If angle closure is already present with increased IOP, pressure lowering topicals should be started with subsequent surgical intervention for refractory glaucoma, preferably after intraocular inflammation has been brought under control. For posterior uveitis, or for severe anterior segment inflammation, systemic or periocular (i.e. subtenon) steroids in combination with a histamine blocker are given. Steroids may be tapered according to response to treatment, with follow up examination and monitoring of IOP every 1-7 days depending on the degree of inflammation and intraocular involvement. Once asymptomatic, patients may be reexamined every 3-6 weeks if still on steroid treatment, and every 3-6 months thereafter. Concurrent referral to an internist is advisable for evaluation of pulmonary and other systemic manifestation of sarcoidosis.
| | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in