|
|
 |
 |
 |
 |
|
|
Orbit/Oculoplastics Quiz 7
|
Printer Friendly
|
|
|
|
[Back to Questions] [Back to Orbit/Oculoplastics]
|

Figure 1
Orbital CT of a forty-eight year old woman with slowly progressive proptosis in the left eye over the past 8 months.
|
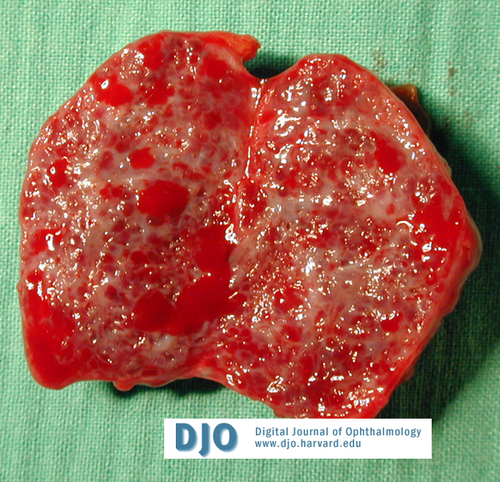
Figure 2.
Surgical specimen.
|
| | Case History | | A forty-eight year old woman presents with a several month history of slowly progressive, painless proptosis and blurred vision in the left eye. She is otherwise healthy. Her examination was notable for choroidal folds OS. | | | Questions and Answers | 1. What is the differential diagnosis of the lesion shown in the scan?
Answer: The lesion is a well-defined, round, intraconal mass in a middle-aged woman, most likely a cavernous hemangioma. These tumors are the most common benign orbital tumors in adults. Additional considerations include schwannoma, fibrous histiocytoma, lymphoma, and venous malformation. Metastatic disease, especially breast cancer, could be considered but would be less likely given the patient's age and good health status.
2. What additional parts of the history and examination are especially pertinent regarding this patient’s presentation?
Answer: Additional history should include inquiries about pain which might suggest hemorrhage in to a vascular malformation. The presence of a pulsatile sensation in the orbit is highly suggestive of an arteriovenous malformation or fistula. Diplopia and episodes of amaurosis are indicative of mass effect in the orbit comprising extraocular muscle and optic nerve function repsectively. It is of paramount importance to fully ascertain whether visual function has been compromised by the mass as this will guide management decisions. The examination should focus on visual acuity, color vision, motility, visual fields, and exophthalmometry.
3. What diagnostic tests are indicated in this case?
Answer: High resolution, multi-view computed tomography with intravenous contrast usually provides the best imaging of these types of lesions. Assessment of tumor composition and neural involvement may be augmented with magnetic resonance imaging. B-scan ultrasonography may be useful if there is a question of orbital extension of an intraocular tumor, but this is usually not necessary. Color Doppler ultrasound can provide in formation regarding the nature of blood flow within the lesion. Serial visual field testing will help monitor clinical progression of the lesion.
4. What are the clinical and histopathologic manifestations of the lesion?
Answer: The most common clinical manifestation of orbital cavernous hemangioma is slowly progressive painless proptosis. Other findings on exam can include a hyperopic shift in the patient’s refraction and strabismus. Posterior segment exam can reveal retinal striae/choroidal folds if the tumor is compressing the globe. Compression may also lead to an increase in intraocular pressure. Optic nerve compression may lead to dyschromatopsia, episodes of gaze evoked amaurosis, and visual field loss.
Cavernous hemangiomas are low-flow encapsulated vascular malformation comprised of ectatic, usually thrombosed venous channels.
5. How would you manage this lesion?
Answer: Surgical excision of cavernous hemangiomas is the treatment of choice for lesions in which visual symptoms or deficits are attributable to the tumor. In the event that visual function is not threatened, observation with serial examination, including visual field testing is acceptable; however, if a tumor appears to be growing (as measured by either exophthalmometry or radiographic imaging) and there is a concern that visual function may be compromised in the future, early excision is likely to be technically less challenging and is also an acceptable option.
| | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in