|
|
 |
 |
 |
 |
|
|
Neuro-ophthalmology Quiz 5
|
Printer Friendly
|



Howard Pomeranz, M.D. | Massachusetts Eye and Ear Infirmary, Harvard Medical School, University of Maryland Medical Center M.A. Afshari, M.D., M.P.H. | Massachusetts Eye and Ear Infirmary, Harvard Medical School August 1, 1997
|
|
[Back to Questions] [Back to Neuro-ophthalmology]
|
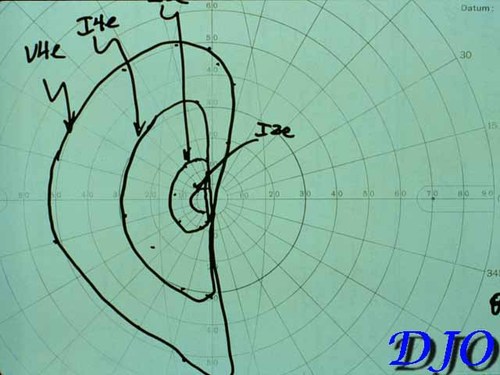
Figure 1
Kinetic Visual Field
|
|
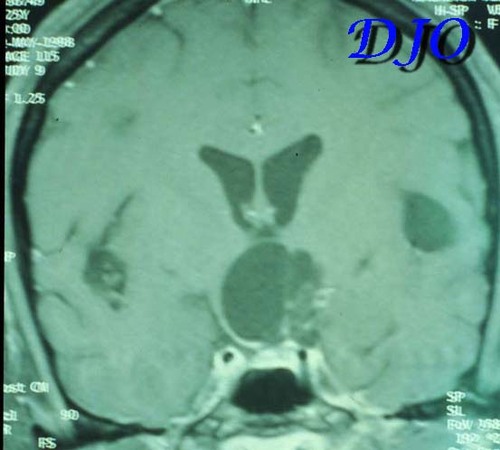
Figure 3
|
| | Case History | A 25 year-old right handed Ecuadorian woman was well until age 20 when she developed seizures. A CT scan of the head revealed calcified cysts in the cerebral cortex. She was treated with tegretol. Twelve months ago she noted the onset of visual loss in her peripheral visual field of the left eye. This visual loss progressed to loss of central vision in the left eye. Two months ago she began to notice loss of peripheral vision in the right eye.
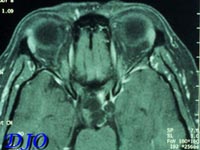
On ophthalmic examination her visual acuity with correction was 20/40 OD and 20/80 OS with no improvement with pinhole. Her color vision was normal bilaterally. There was no evidence of proptosis, ptosis, afferent pupillary defect or ocular motility deficits. Anterior segment exam and intraocular pressures were normal. Kinetic visual field is shown below. Fundus exam revealed myopic optic nerves and temporal pallor of the left optic nerve. A magnetic resonance scan of the head was obtained. Axial and coronal sections are shown below.
References:
Keane, JR. Neuro-ophthalmic signs and symptoms of cysticercosis. Arch Ophthalmol 1982; 100: 1445-1448.
Grisolia JS and Wiederholt WC. CNS cysticercosis. Arch Neurol 1982; 39: 540-544.
McCormick GF, Zee CS and Heiden J. Cysticercosis cerebri: review of 127 cases. Arch Neurol 1982; 39: 534-539.
Odel JG and Moazami G. Diseases caused by helminths. In Walsh and Hoyt's Clinical Neuro-ophthalmology Vol. 4, fifth edition. NR Miller and NJ Newman, eds. Baltimore: Williams and Wilkins; 1998: 4460-4479. | | | Questions and Answers | 1. What is this patient's most likely diagnosis?
Answer: Neurocytsticercosis. Cysticercosis is common in Mexico, Central and South America as well as other parts of the world. Neurocysticercosis is the most common parasitic disease of the central nervous system and is the single most common cause of late-onset seizures in both adults and children in Mexico and several other developing countries. Parenchymal neurocysticercosis occurs when cysticerci develop within the brain. Patients with this form of the disease can present with seizures, alterations of mental status and focal neurologic deficits including hemiplegia, quadriplegia, hemisensory loss, aphasia and ataxia. Subarachnoid neurocysticercosis is characterized by signs and symptoms of meningitis and increased intracranial pressure including headache, nausea, neck stiffness, seizures, papilledema, secondary optic atrophy and cranial neuropathies. Location of a cyst in the sella turcica may produce endocrine symptoms that mimic a primary pituitary tumor. Extension of the cyst INTO the suprasellar cistern may produce decreased vision in one or both eyes associated with chiasmal field defects FROM compression of the intracranial optic nerves and the optic chiasm. Intraventricular neurocysticercosis due to obstruction of one or more ventricles by a cyst may lead to hydrocephalus. Cysts may also be located beneath the conjunctiva, in the eyelid, in the extraocular muscles, within the orbital muscle cone or within the eye itself.
2. What portion of the anterior visual system is most likely affected?
Answer: The bitemporal visual field defect would be suggestive of chiasmal involvement of the anterior visual pathway. The coronal section of the brain through the region of the chiasm shows compression of the chiasm by a suprasellar cysticercosis cyst.
3. What other neuro-ophthalmic problems can arise in patients with this diagnosis?
Answer: Neuro-ophthalmic manifestations of neurocysticercosis include homonymous visual field defects, cortical blindness, optic neuropathy, papilledema, nystagmus, ocular motor dysfunction FROM damage to intrinsic pathways for ocular motor control within the brain stem and cranial nerve pareses including ocular motor, trigeminal and facial nerves.
| | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in