|
|
 |
 |
 |
 |
|
|
General Ophthalmology Quiz 11
|
Printer Friendly
|



Yichieh Shiuey, MD | Massachusetts Eye and Ear Infirmary, Harvard Medical School June 1, 1998
|
|
[Back to Questions] [Back to General Ophthalmology]
|
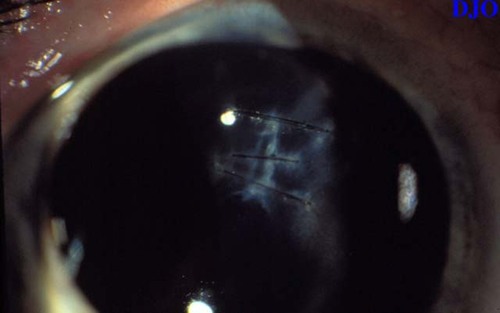
Figure 1
Figures 1-2. These are the slitlamp photographs of a young man with a history of a corneal laceration and traumatic cataract due to a high speed metallic foreign body. He underwent simultaneous corneal laceration repair, phacoemulsification, and placement of a posterior chamber sulcus fixated lens. Two months after presentation his vision in this eye was 20/20 with spectacle correction.
|

Figure 2
|
| Questions and Answers | 1. What radiologic studies would be helpful in the initial evaluation of a patient with a suspected metallic intraocular foreign body?
Answer: Plain films are best to detect the presence or absence of a metallic intraocular foreign body, but are not very precise at localization. Computed tomography using 1 mm cuts in both the axial and coronal planes is ideal for precise localization of foreign bodies.
2. What types of prophylaxis against infection should be considered in a patient with an open globe injury?
Answer: Tetanus toxoid should be given to all patients with an open globe, who do not have clear documentation of their tetanus immunization status. Systemic antibiotics should be considered for prophylaxis of traumatic endophthalmitis. At the Massachusetts Eye and Ear Infirmary patients with open globe injury are routinely given intravenous vancomycin and ceftazadime for 48 hours. This antibiotic regimen is designed to cover bacillus species, gram positive cocci, pseudomonas, and other gram negative organisms.
3. When should primary removal of a traumatic cataract be considered?
Answer: Traumatic cataracts produced by laceration of the lens capsule and which are associated with flocculent lens material should be removed at the time of open globe REPAIR to reduce the risk of excessive inflammation FROM phacoanaphylaxis. Traumatic cataracts with intact lens capsules that have been produced by blunt injury should usually be removed secondarily.
4. When can simultaneous REPAIR of corneal laceration, removal of traumatic cataract, and placement of a PCIOL be considered?
Answer: Small case series have shown that the patients that do best with simultaneous REPAIR of corneal laceration, removal of traumatic cataract, and placement of a PCIOL have the following characteristics: 1) Absence of posterior segment injury 2) A clean appearing corneal wound 3) Adequate visualization of the lens after REPAIR of the corneal laceration 4) Adequate capsular support for intracapsular or sulcus placement of the PCIOL
5. When should sutures FROM the corneal laceration wound be removed?
Answer: Sutures can be removed between 6 and 12 weeks after the time of initial REPAIR based on the appearance, keratometry, and computerized videokeratography.
| | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in