|
|
 |
 |
 |
 |
|
|
Retina/Uveitis Quiz 23
|
Printer Friendly
|
|
|
|
[Back to Questions] [Back to Retina/Uveitis]
|
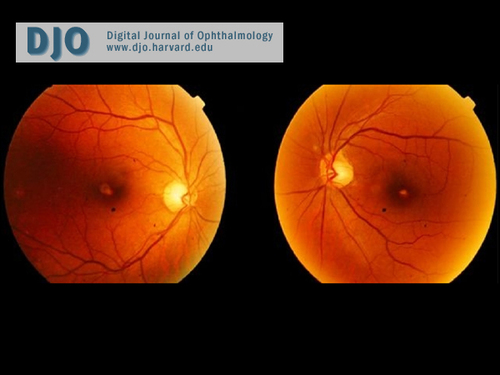
Figure 1
Fundus photographs of the right and left eyes.
|

Figure 2
Optical coherence tomography (OCT) of the right eye (above) and left eye (below) showing attenuation of the neurosensory retina with foveal thinning.
|

Figure 3
Fluorescein angiogram of the right eye showing arterio-venous phase with window defect.
|
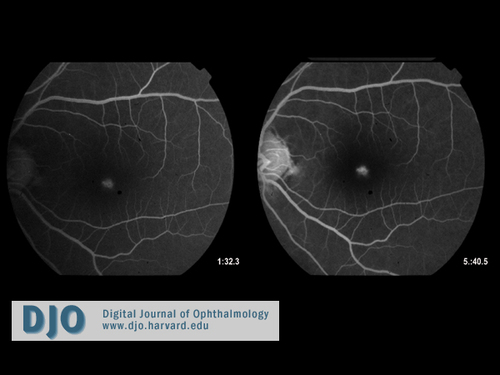
Figure 4
Fluorescein angiogram of the left eye showing a window defect.
|
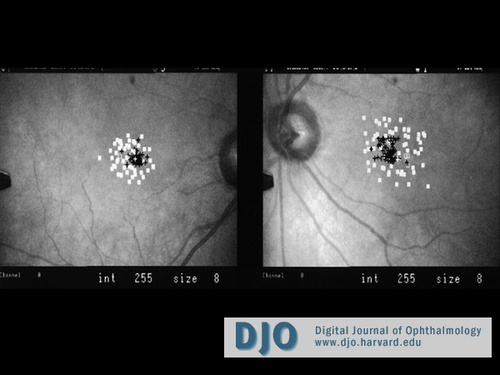
Figure 5
Scanning Laser Ophthalmoscope (SLO) microperimetry. Black cross indicates fixation. Empty boxes show a few small scotomata bilaterally.
|
| | Case History | | A healthy 65-year-old man was seen for a routine eye exam and referred to the retina service due to the fundus findings shown in Figure 1. Uncorrected visual acuity was 20/40 with pinhole improvement to 20/25 OU. The external examination was normal. Anterior segment examination was unremarkable except for 1+ nuclear sclerosis bilaterally. | | | Questions and Answers | 1. What is the differential diagnosis?
Answer: Macular hole, chloroquine/hydroxychloroquine toxicity, age-related macular degeneration, adult foveomacular dystrophy, Best’s disease, Stargardt disease, rod-cone dystrophy, benign concentric macular dystrophy, phototoxicity after bilateral intraocular surgery, and solar retinopathy.
2. What further questions would you like to ask the patient?
Answer: A thorough history is essential in narrowing the list of possible diagnoses. Does the patient have any vision problems? When did the vision problems start? What medications has the patient been on? Is there a family history of vision problems? Has the patient had any eye surgeries in the past? Is the color vision affected? Does the patient have a history of sun gazing?
On further questioning, this patient reported having difficulty reading fine print for the last two months even with reading glasses. He also acknowledged being a “sun-gazer for more than 40 years.” However, during the past 6-8 months, he had changed his sungazing routine from sunrise and sunset to noon. Of note, the patient had a normal fundoscopic examination three years earlier, including normal foveal light reflexes.
3. What is the most likely diagnosis, and what is it associated with?
Answer: Solar retinopathy. Most cases are associated with observation of a solar eclipse, but it has also been described in psychiatric patients, sailors, military recruits, and sungazers for personal or religious rituals. (1,2)
A macular hole is not noted on the OCT (Figure 2). Additionally, there is no evidence of lipofuscin deposits in the outer retinal layers eliminating the diagnosis of adult foveo-macular dystrophy. The patient’s visual symptoms started in the sixth decade of his life, and he still has good vision ruling out the atrophic stage of Best disease. There is no history of past use of chloroquine or hydroxychloroquine. There is no evidence of drusen or fish-like flecks on the fundus photographs, fluorescein angiography (Figures 3 and 4), or OCT; thus, the diagnosis of age-related macular degeneration and Stargardt’s disease are eliminated. The patient has not undergone any ocular surgery in the past to consider phototoxicity. Although the OCT findings in rod-cone disease and benign concentric macular dystrophy can be similar to the OCT of this patient, the patient has no night vision or color vision problem, and the fundus photograph shows no attenuation of the arteries and no pallor of the optic nerve. Therefore, the diagnosis of cone-rod disease is unlikely. Electroretinography can be used to confirm this. Benign concentric macular dystrophy is characterized by an annular hypopigmented area around the foveola with central sparing as well as a hyperreflective and thick RPE in the area of pigmentation on OCT. These signs are not seen in the fundus photos or OCT above.
4. What are the symptoms?
Answer: Patients can have a noticeable scotoma or decreased visual acuity. In some cases the visual acuity may be unaffected but patients might have minute scotomas, which they may or may not readily appreciate.
5. What are the findings in solar retinopathy?
Answer: Fundus exam shows a small, yellow foveolar spot during the acute phase of the injury. In later stages, a pseudolamellar macular hole-like lesion may be seen with a perifoveal ring of RPE depigmentation (Figure 1). OCT findings in both acute and chronic solar retinopathy have been described.(3,4) One study described increased reflectivity in all retinal layers of the fovea without evidence of macular edema 48 hours after injury. These findings were reversible on repeat OCT.(3) OCT findings of chronic solar retinopathy, as seen in this case, show attenuation of the neurosensory retina with foveal thinning (Figure 2) and a hyporeflective space at the level of outer retina and retinal pigment epithelium.(4) Fluorescein angiography can be normal or may show a window defect (Figure 3 and 4). Scanning laser ophthalmoscope (SLO) microperimetry may reveal few minute central scotoma and can be used in subtle cases of solar retinopathy (Figure 5).
6. What is the pathophysiology?
Answer: The mechanism of injury to the retina from solar radiation has been suggested to be a combination of thermal and photochemical damage to the photoreceptors and RPE.(5) The retina, especially the fovea, is susceptible to injury from visible blue light and ultraviolet radiation. Histopathologic findings include degeneration of the RPE cells characterized by loss of plasma membrane specialization and swelling of the smooth endoplasmic reticulum. Examination of photoreceptor cells demonstrates mitochondrial swelling, nuclear pyknosis, and fragmentation of the photoreceptor lamellae.(5)
This particular case of solar retinopathy shows some of the classic findings of solar retinopathy as seen on various imaging modalities. However, it is unusual that even though the patient had a decades-long history of sun gazing, he did not have any clinical evidence or symptoms of solar retinopathy until after he started sun gazing at noon. This suggests that the intensity of UV rays falling in the fovea may be more damaging than the length of exposure. Yannuzzi et al. have reported several cases of solar retinopathy in patients who were sunbathing at noon on a clear day but had no history of direct sun gazing. Retinal irradiance from reflected light off the water may have been the culprit.(6) The authors suggest various geophysical factors may have played a role in causing phototoxicity such as exposure at solar noon and the possible increase in UV-B radiation by relatively low ozone layer in the particular geographic areas. Patients who are emmetropes may also be more susceptible to foveal damage since light is focused sharply on the fovea in these patients.(6)
References:
1. Hope-Ross M, Travers S, Mooney D. Solar retinopathy following religious rituals. Br J Ophthalmol 1988;72: 931-934 .
2. Codenotti M, Patelli F, Brancato R. OCT findings in patients with retinopathy after watching a solar eclipse. Ophthalmologica 2002; 216: 463–466.
3. Bechmann M, Ehrt O, Thiel MJ et al., Optical coherence tomography findings in early solar retinopathy. Br J Ophthalmol 2000; 84: 547–548.
4. Garg SJ, Martidis A, Nelson ML, Sivalingam A. Optical coherence tomography of chronic solar retinopathy. Am J Ophthalmol 2004; 137: 351-354.
5. Hope-Ross MW, Mahon GJ, Gardiner TA, Archer DB. Ultrastructural findings in solar retinopathy. Eye 1993; 7: 29-33.
6. Yannuzzi LA, Fisher YL, Krueger A, Slakter J. Solar Retinopathy: A Photobiological and Geophysical Analysis. Trans Am Ophthalmol Soc 1987; 85: 120-158. | | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in