|
|
 |
 |
 |
 |
|
|
Cornea/Refractive Surgery Quiz 25: A 61-year-old man with a complication of intraocular surgery
|
Printer Friendly
|


 Tarek Alasil
Tarek Alasil | Doheny Eye Institute, University of Southern California Michael Engelbert | Edward S. Harkness Eye Institute, lumbia University Lama A. Al-Aswad | Edward S. Harkness Eye Institute, Columbia University September 5, 2008
|
|
[Back to Questions] [Back to Cornea/Refractive Surgery]
|
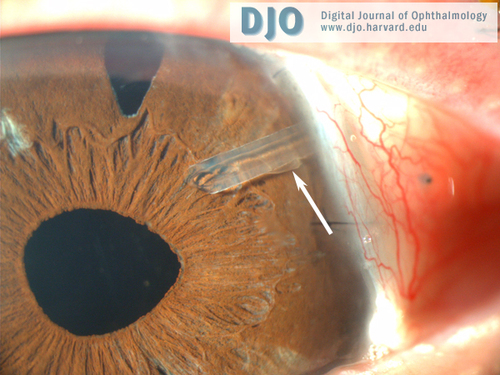
Figure 1
Slit-lamp examination of the left eye shows an iatrogenic Descemet’s membrane tear (arrow). There is no corneal edema noted.
|

Figure 2
Anterior segment optical coherence tomography of the left eye showed the Ahmed valve tube and iatrogenic Descemet’s membrane tear. There is no corneal edema noted.
|
| | Case History | | A 61-year-old man with advanced open angle glaucoma and visually significant cataracts underwent combined cataract extraction, intraocular lens implantation, and Ahmed valve placement in the left eye. Six weeks later, the patient was evaluated in the clinic for a routine follow-up. The slit-lamp exam and anterior segment optical coherence tomography done at that time are shown below. | | | Questions and Answers | 1. What condition does this patient have?
Answer: The patient has an iatrogenic Descemet’s membrane tear that is seen on slit-lamp examination (Figure 1; arrow) and anterior segment optical coherence tomography (Figure 2). There was no corneal edema noted.
2. How did the patient develop this condition, and what is its clinical significance?
Answer: The patient likely developed the Descemet's membrane tear as a complication of cataract surgery (iatrogenic). A Descemet's membrane tear can progress into a detachment, which is a potentially devastating complication of cataract surgery. Small localized detachments are rarely problematic. Persistent extensive detachments, however, can compromise visual acuity by causing corneal edema, decompensation, and scarring.(1)
3. At which point during glaucoma or cataract surgery can the Descemet's membrane be torn or stripped?
Answer: In some patients the attachment between Descemet's membrane and the underlying stroma is less sturdy and may be more prone to tears. Generally, tears occur when dull blades are used. Instead of sharply incising Descemet's, some surgeons will accidentally catch it and push it causing a tear. Dull blades can also leave rough edges of the membrane, which can then be caught by the phaco tip or other instrumentation as it passes in and out of the main incision or paracentesis. This can happen while placing the tube of the Ahmed valve into the anterior chamber. Once the edge of Descemet's membrane has torn, irrigating fluid or viscoelastic can easily track under the membrane and create a total detachment.(2)
4. How could the Descemet’s tear be managed intraoperatively in order to avoid further stripping of the membrane?
Answer: If a piece of the membrane is caught, the careful placement and removal of instruments becomes critical for the remainder of the procedure. Every time an instrument is inserted and removed from the incision, it should be turned away from the area of detachment in order to avoid the continual catching or further stripping of the membrane anterior to the incision. Be sure the phaco tip is well into the anterior chamber before applying irrigation so that irrigating fluid does not get under Descemet's membrane. Also, inject viscoelastic only when the canula tip is well beyond the incision. The same care must be taken through the paracentesis.(2)
5. What should be done when closing the incision, and why?
Answer: When closing the incision, slightly overfill the chamber with BSS. A small amount of pressure on either the main incision or the paracentesis will create a current that will wash any scrolled Descemet's membrane into the normal position at the incisional site. This will also place the membrane tightly against the underlying stroma and allow the endothelium "to pump it back into place." If the membrane does not maintain its position against the stroma, it may require suturing. The sutures should be placed through the Descemet's detachment and the remaining cornea in order to pull the membrane into place. Then an air bubble can be used to tamponade the membrane against stroma.(2)
6. What other modalities can be considered for fairly large Descemet’s detachments?
Answer: Intracameral injection with either sulfur hexafluoride (SF6) or perfluoropropane (C3F8) gas has gained increasing acceptance as an efficient and effective treatment option for Descemet membrane detachments after cataract surgery.(3, 4) No corneal decompensation or fluctuations in intraocular pressure were believed to be attributable to isoexpansile gas exchange.(5) In severe cases, where persistent extensive Descemet detachments can affect visual acuity, penetrating keratoplasty (full-thickness corneal grafting) may be required for restoration of vision.(1)
7. How does gas treat a Descemet’s detachment?
Answer: The gas may be used at the time of surgery or afterward if a detachment is noted postoperatively. Gas is injected into the anterior chamber to almost fill it. Then the patient should be monitored on an hourly basis. The gas must be allowed to expand and raise the pressure of the eye up to about 40 mm Hg. This gas will tamponade Descemet's membrane up against the stroma, where the endothelial pump will hold it. When the pressure hits 40 mm Hg, release enough gas through the paracentesis to drop the intraocular pressure to a normal level. This must be repeated 1-2 times per day. By day's end, 50-60 percent of the bubble should have been released to ensure that the intraocular pressure does not increase overnight. This method may be used for one to seven days postoperatively.(2)
References:
1. Nouri M, Pineda R Jr, Azar D. Descemet membrane tear after cataract surgery. Semin Ophthalmol. 2002 Sep-Dec;17(3-4):115-9.
2. William J. Fishkind. Facing Down the 5 Most Common Cataract Complications. Review of Ophthalmology. Oct 2001.
3. Kim T, Hasan SA. A new technique for repairing descemet membrane detachments using intracameral gas injection. Arch Ophthalmol. 2002 Feb;120(2):181-3.
4. Gault JA, Raber IM. Repair of Descemet's membrane detachment with intracameral injection of 20% sulfur hexafluoride gas. Cornea. 1996 Sep;15(5):483-9.
5. Macsai MS, Gainer KM, Chisholm L. Repair of Descemet's membrane detachment with perfluorpropane. Cornea. 1998;17:129-134. | | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in