|
|
 |
 |
 |
 |
|
|
Orbit/Oculoplastics quiz 23: A sixty year-old man with unilateral proptosis
|
Printer Friendly
|


 Ann-Marie Lobo, MD
Ann-Marie Lobo, MD | Massachusetts Eye & Ear Infirmary and Harvard Medical School Sureka Thiagalingam | Massachusetts Eye and Ear Infirmary Calliope Allen | Massachusetts Eye and Ear Infirmary May 20, 2007
|
|
[Back to Questions] [Back to Orbit/Oculoplastics]
|

Figure 1
The patient displaying unilateral proptosis
|

Figure 2
Axial CT scan of a patient with unilateral proptosis
|
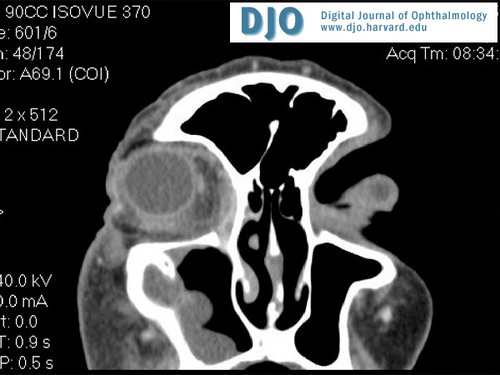
Figure 3
Coronal CT scan showing sinus disease and orbital inflammation
|
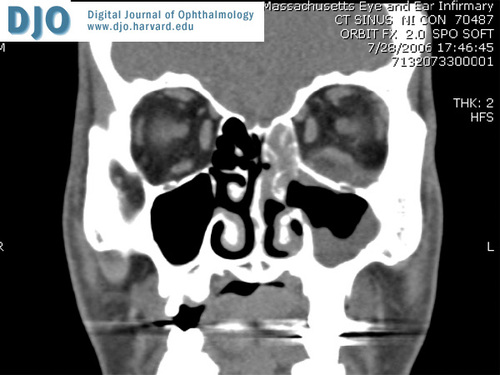
Figure 4
Coronal CT scan of a diabetic patient with orbital extension of sinus disease found to be mucormycosis.
|
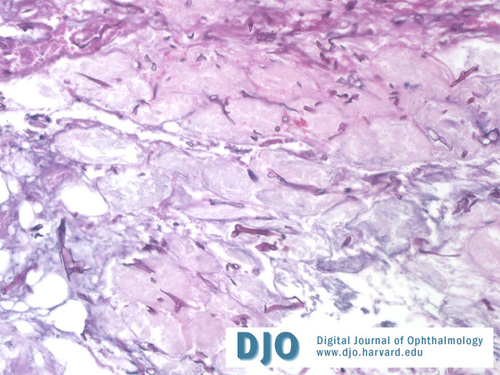
Figure 5
Pathology of orbital lesion demonstrating branching hyphae.
|
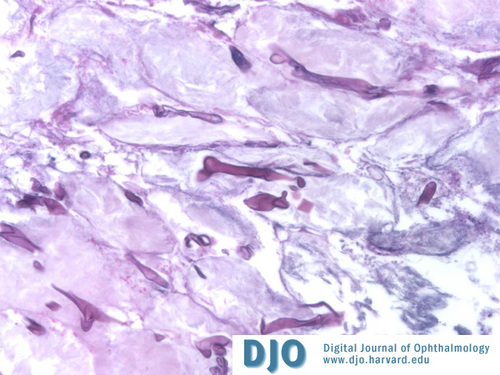
Figure 6
Higher magnification of orbital pathology: branching non-septated hyphae.
|
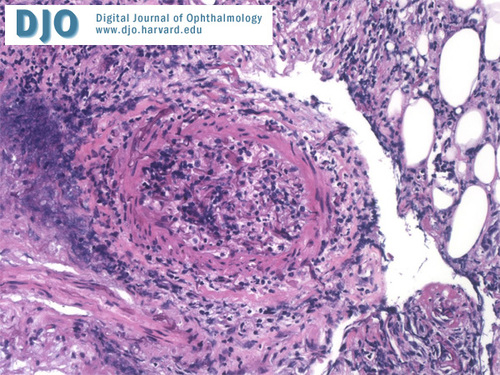
Figure 7
Invasion of vessel by hyphae and inflammatory cells.
|
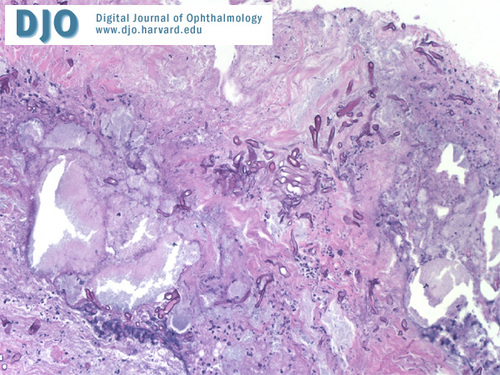
Figure 8
Hyphae within sinus mucosal tissue.
|
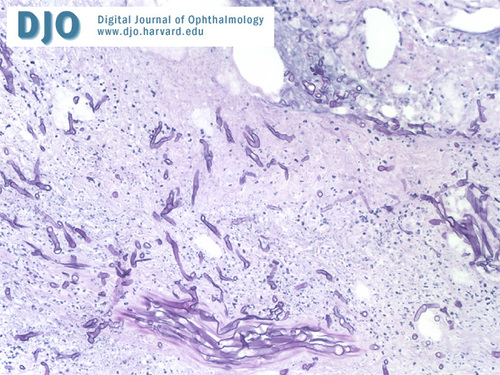
Figure 9
Nonseptated hyphae within necrotic sinus tissue.
|
| | Case History | | A sixty year-old man with lymphoma presents with unilateral proptosis. | | | Questions and Answers | 1. What is the differential diagnosis?
Answer: The differential diagnosis of unilateral proptosis in an immunocompromised patient includes bacterial orbital cellulitis, preseptal cellulitis, idiopathic orbital inflammation, inflammation around a metastatic lesion within the orbit, thyroid related orbitopathy, orbital tumor, or invasive fungal infection.
Mucormycosis or zygomycosis is an invasive fungal infection from the family Mucoraceae, which includes the Mucor, Rhizopus, and Absidia subtypes. These saprophytic fungi can be found in common decaying foods. Spores are inhaled and are cleared by phagocytosis in healthy patients; however, in immunocompromised hosts, these spores can germinate with the development of hyphae in the oral and sinus mucosa. Hyphae may invade the elastic lamina of blood vessels with subsequent development of thrombosis and tissue necrosis. This necrotic environment facilitates further growth of fungi and may lead to extension of the infection into orbital and intracranial tissues (also known as rhino-orbito-cerebral mucormycosis). Mucormycosis has commonly been classified as an opportunistic infection, specifically affecting patients with diabetes (especially in ketoacidosis), lymphoma, renal failure, and other immunocompromised states. Mucormycosis has also been known to affect patients with diseases associated with iron overload such as hemochromatosis and multiple blood transfusions; the fungus utilizes iron as a growth factor. Similarly, mucormycosis has been found in patients on desferroxamine therapy because the desferroxamine provides the chelated form of iron that these fungi can utilize for growth. There have been several reports of cases of mucormycosis in immunocompetent patients.
2. What are characteristic signs on exam?
Answer: Patients may present with complaints of edema, facial/periorbital pain, diplopia, and vision loss. Orbital signs of mucormycosis include proptosis, chemosis, periorbital edema, vision loss, and ophthalmoplegia (Figure 1). A classic late finding on exam of the nasal septum is a black eschar which results from the ischemic infarction and septic necrosis of tissues invaded by hyphae.
3. What types of diagnostic tests should be done to confirm the diagnosis?
Answer: Diagnostic tests include a complete ophthalmologic exam and evaluation of the nose and sinuses for signs of active infection/inflammation or necrotic tissue. Imaging may be performed to further delineate the source of infection, degree of sinus involvement, and amount of extension into other tissues, although early in the disease there may only be mild mucosal thickening of the sinuses (see figures 2-4). Imaging may also help with treatment decisions such as conservative local debridement versus orbital exenteration.
Definitive diagnosis is made based on fungal culture data and histopathology of nasal or orbital tissue with characteristic thick, nonseptated hyphae branching at right angles (see figures 5-9). Biopsy of nasal mucosa for diagnosis should be done on both suspicious and normal appearing mucosa since the classic eschar is a late finding and normal appearing mucosa may harbor organisms.
4. What are the options for treatment and further management of this condition?
Answer: If the diagnosis of mucormycosis is presumed based on clinical exam of the nose/orbit and histopathology confirms the presence of hyphae in sinonasal tissues or orbital tissue, treatment with intravenous antifungals should be implemented immediately. The primary antifungal treatment is intravenous amphotericin B, although other antifungal agents have been used in patients who cannot tolerate amphotericin B. The liposomal form of amphotericin B has allowed for an improved therapeutic index and a decrease in overall toxicity of the drug.
Although antifungal agents are important in the treatment of mucormycosis, the primary treatment is extensive surgical debridement of the involved tissues. Serial debridements may be done with frozen section monitoring to ensure surgical margins are clear of fungal infection. Depending on the degree of orbital involvement and the age/visual prognosis of the patient, exenteration of necrotic tissues can be performed to prevent further intracranial extension of infection.
Because of the poor prognosis associated with mucormycosis, other experimental treatments have been explored. A few case reports have demonstrated the benefits of other therapies including local irrigation and infusion of debrided tissues with amphotericin B. Because of the ischemic, necrotic environment caused by fungal invasion of blood vessels, local intraconal injections or packing with antifungal agents may provide more penetrance and better efficacy than systemic therapy alone. Adjunctive treatment with hyperbaric oxygen therapy has also been used in patients with mucormycosis with the idea that high concentrations of oxygen may reduce the acidotic environment in which fungi grow and invade. High oxygen concentrations may also inhibit further growth of the fungi.
For diabetic patients, treatment also includes correction of underlying metabolic abnormalities such as ketoacidosis. Overall, mortality rates tend to be lower in diabetic patients compared to other immunosuppressed patients. Early diagnosis and treatment is essential in the management of mucormycosis. Delayed diagnosis can lead to poor outcomes and increased mortality.
Pathology photographs courtesy of Dr. Sureka Thiagalingam
References:
Hargrove, RN, Wesley, RE, Klippenstein, KA, et al. Indications for orbital exenteration in mucormycosis. Ophthalmic Plastic and Reconstructive Surgery 2006;22(4):286-291.
Nithyanandam, S, Jacob MS, Battu RR, et al. Rhino-orbito-cerebral mucormycosis: a retrospective analysis of clinical features and treatment outcomes. Indian Journal of Ophthalmology 2003;51(3):231-236.
Pelton, RW, Peterson, EA, Patel, BCK, and Davis, K. Successful treatment of rhino-orbital mucormycosis without exenteration. Ophthalmic Plastic and Reconstructive Surgery 2001;17(1): 62-66.
Peterson, KL, Wang, M, Canalis, RF, and Abemayor, E. Rhinocerebral mucormycosis: evolution of the disease and treatment options. The Laryngoscope 1997;107:855-862.
Price, JC and Stevens, DL. Hyperbaric oxygen in the treatment of rhinocerebral mucurmycosis. The Laryngoscope 1980;90:737-747.
Talmi, YP, Goldschmied-Reoven, A, Bakon, M, et al. Rhino-orbital and rhino-orbito-cerebral mucormycosis. Otolaryngology – Head and Neck Surgery 2002; 127(1):22-31.
| | | [Back to Questions] |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in