|
|
 |
 |
 |
 |
|
|
A 65-year-old man with decreased vision OD
Digital Journal of Ophthalmology 2008
Volume 14, Number 11
June 15, 2008
|
Printer Friendly
|
|
|
|
|
|
|
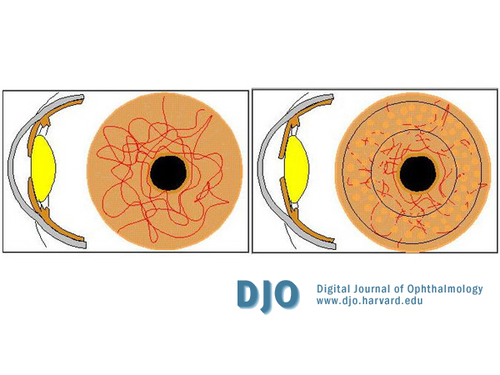
| Treatment | The patient received intravenous, oral and topical anti-glaucoma medications to reduce the IOP. Topical steroids were started to reduce intraocular inflammation. A 360-degree laser iridoplasty was performed to tighten the iris, open up the angles of the anterior chamber and ablate the NVI (Figure 3). A laser iridotomy was performed to facilitate drainage of aqueous from the eye. Extensive pan-retinal photocoagulation (PRP) was carried out to reduce the oxygen requirement of the peripheral retina and the hypoxic drive for angiogenesis. The patient declined carotid endarterectomy (CEA).
Despite the above treatment and maximum topical anti glaucoma medication over the next 8 months, the NVI failed to regress and the IOP gradually increased to 50 mm Hg. The eye, however, remained comfortable. The left eye was unaffected.
The patient was lost to follow-up for 4 months. He then presented to the casualty service with complaints of recurrent episodes of sudden, painless loss of vision in the left eye for one week. He reported that the vision usually returned to normal within a few minutes to half an hour. There was no associated headache, neck pain, myalgia, jaw claudication (suggestive of giant call arteritis) or nausea and vomiting.
On examination, his blood pressure was within normal limits. Visual acuities were no light perception (NLP) OD and 20/40 OS. He had bilateral cataracts (mature in OD), severe NVI and high IOP (50 mm Hg OU). The left eye showed advanced optic disc cupping with visible spontaneous retinal arterial pulsation. The right fundus was not visualised due to a dense cataract.
His treatment was similar to that given for the right eye; specifically, he received intravenous, oral and topical anti-glaucoma agents, topical steroids, argon-laser iridoplasty, Nd:Yag laser iridotomies and extensive PRP.
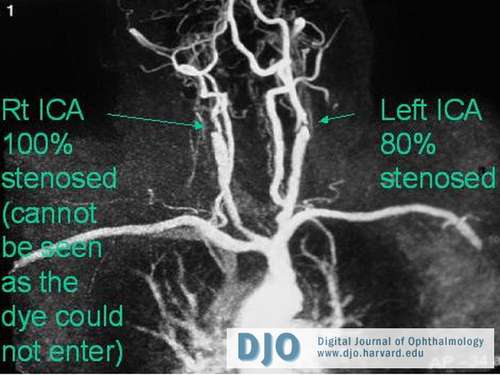
Carotid angiography revealed 100% stenosis of right internal carotid artery and 80% stenosis of left internal carotid at its origin (Figure 4). He was advised to stop smoking and was offered carotid endarterectomy with 50% risk of major complications such as stroke or death. The patient elected to proceed and had successful surgery with a saphenous vein patch.
Post-operatively, his IOP OS remained at 50 mm Hg along with intermittent visual obscurations and visible central retinal arterial pulsations. Accordingly, trabeculectomy was performed with Mitomycin C (0.2mg/ml) and two releasable sutures. A surgical peripheral iridectomy was not fashioned due to the risk of hemorrhage from the florid NVI; intentionally a large Nd:YAG peripheral iridotomy was positioned immediately beneath the bleb.
On follow up examination, both eyes were comfortable. Visual acuity OS was 20/63 with an IOP of 10 mm Hg without anti glaucoma medication. Visual acuity OD remained NLP with an IOP of 55 mm Hg despite ongoing treatment with topical prostaglandin analogues (Latanoprost 0.005%), alpha-2 agonist (Brinzolamide 1%) and beta blocker (Timolol 0.5%). | |
|
Figure 3
360-degree Argon laser iridoplasty to tighten the iris, open up the angles of the anterior chamber and ablate the NVI
 |
|
|
Figure 4
Carotid angiography showed 100% stenosis of right internal carotid artery and 80% stenosis of left internal carotid at its origin
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in