|
|
 |
 |
 |
 |
|
|
An 89-year-old man with acute vision loss in the right eye
Digital Journal of Ophthalmology 2007
Volume 13, Number 6
February 10, 2007
|
Printer Friendly
|
|
|


 Annette Sims
Annette Sims | University of South Florida Burton Goldstein | University of South Florida
|
|
|
| Examination | On examination, the visual acuity was count fingers in the right eye and 20/30 in the left eye. There was no prior documented visual acuity but he endorsed that the vision in his right eye was previously good. His anterior segment exam was normal. On fundus examination, the right eye had a subretinal hemorrhage with a small intraretinal and pre retinal component approximately two disk diameters involving the center of the macula. His left eye showed minimal pigmentary changes in the macula. A fluorescein angiogram was requested, however, the patient was unable to stay for this test due to transportation issues.
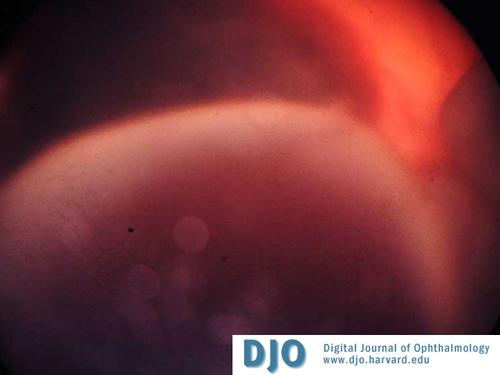
Because of his age, history of hypertension and systemic vasculopathy, macroaneurysm and macular degeneration were considered as likely causes of the macular bleeding. On follow up examination, his condition remained stable and pneumatic translocation of the hemorrhage was offered to the patient. Considering his good visual acuity in the left eye and fear of complication from the procedure, he declined the intervention. Two weeks later the patient returned to clinic complaining of worsening vision and pain in the right eye. The intraocular pressure in the right eye was 27 and there was an inferior hemorrhagic choroidal detachment present (Figure 1). The patient was started on intraocular pressure lowering agents and anti-inflammatory drops. Ten days later the patient returned with severe eye pain and an intraocular pressure of 64. The retina could not be viewed due to vitreous hemorrhage.
| |
|
Figure 1
Right eye with inferior choroidal hemorrhage
 |
|
|
Figure 2
Extensive periorbital hemorrhage tracked subcutaneously down the right side of the patient's face
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in