|
|
 |
 |
 |
 |
|
|
A 57-year-old woman with periocular pain
Digital Journal of Ophthalmology 2021
Volume 27, Number 3
September 3, 2021
|
Printer Friendly
Download PDF |
|
|



Bryan Strelow, MD, MA | Department of Ophthalmology, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Michelle Nguyen, BS | School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Meredith R. Klifto, MD | Department of Ophthalmology, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina
|
|
|
| Treatment | The patient was diagnosed with primary angle closure syndrome. In the setting of headaches, elevated IOP, narrow angles with patent LPIs, gonioscopic peripheral anterior synechiae and AS-OCT suggestive of plateau iris configuration, the decision was made to perform argon laser peripheral iridoplasty (ALPI). Three days following ALPI in both eyes, IOP decreased in each eye (left eye, 20 to 17 mm Hg; right eye, 27 to 18 mm Hg), and AS-OCT demonstrated mild improvement in iris configuration (Figure 2C-D). The patient was then scheduled for routine follow-up in 2 months for IOP monitoring.
One month later, the patient returned to the outpatient urgent care clinic for worsening headache. Her IOP was within normal limits in each eye, and examination revealed no change suggestive of acute angle closure or other acute ophthalmic disease. She was referred to the Emergency Department for further work-up of her severe headache symptoms. She continued to present emergently for severe headache over the next several months. Computed tomography (CT) of the head with and without contrast revealed no intracranial abnormalities. In addition, CT angiography was normal. Labs, including complete blood count, comprehensive metabolic panel, urine analysis, and urine pregnancy tests were all unremarkable. In the Emergency Department, the patient’s symptoms eventually resolved with intravenous fluids and pain medication, including ketorolac.
The patient then returned for delayed ophthalmology follow-up in the glaucoma clinic 7 months after ALPI, when she demonstrated stable IOP in each eye and unchanged examination. The continued headache symptoms were thought to be less likely related to primary angle closure syndrome given the quality of the symptoms and stability of her examination; however, atypical presentation of angle closure was not ruled out. The patient was scheduled for close follow-up at 2 months, with repeat OCT RNFL imaging.
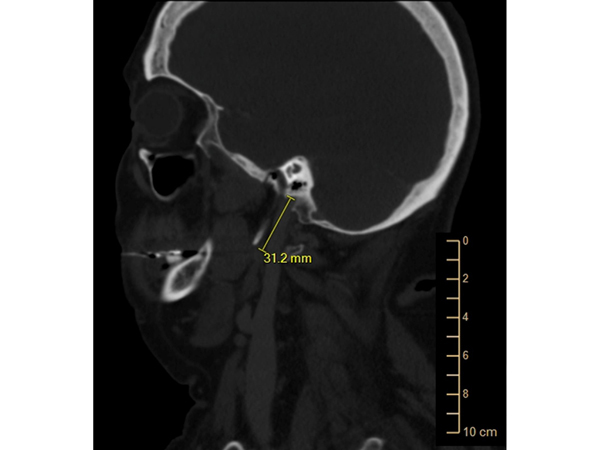
In the course of her continued multidisciplinary workup for her headache symptoms, the patient was referred to otorhinolaryngology, where she received a CT scan of the face and neck, which demonstrated calcification of the stylohyoid ligament (Figure 3). Otorhinolaryngology diagnosed the patient with Eagle syndrome and attributed the recurrent periorbital pain and headaches to this phenomenon. They recommended the patient for stylohyoidectomy.
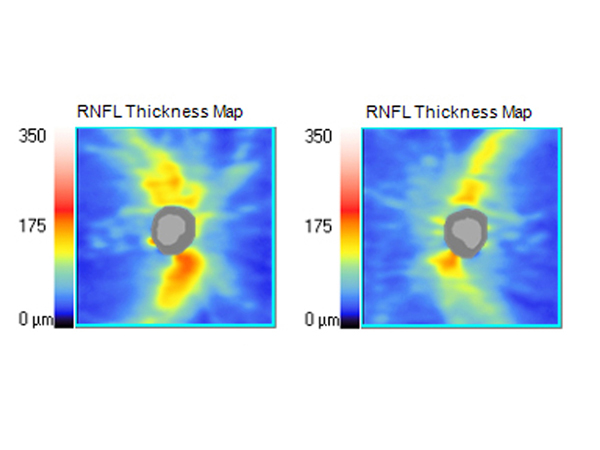
The patient then returned to scheduled 2-month glaucoma follow-up, at which point her OCT testing demonstrated progression of inferior and superior RNFL thinning in the left eye in spite of stable IOPs (Figure 4). Her diagnosis was changed from primary angle closure syndrome to primary angle closure glaucoma. Therapeutic options were discussed with the patient, including medical management with topical eyedrops versus surgical management with cataract extraction. In spite of the provider’s preference for a trial of medical therapy, the patient opted to proceed with cataract extraction. As evidenced by the EAGLE Study, which demonstrated the efficacy and cost-effectiveness of clear-lens exchange as primary treatment for primary angle closure glaucoma, cataract extraction with insertion of intraocular lens was performed along with goniosynechiolysis in the left eye, followed after three weeks by the right eye.(1)
Shortly following these surgeries, the patient underwent trans-oral styloidectomy. On postoperative week 4 after right eye surgery, IOP was 18 mm Hg in each eye, and the patient reported slight lessening of periocular pain. The patient continues to follow-up every 6 months in the glaucoma clinic, with stable IOPs and visual fields off of pressure-lowering eye drops. Overall, after styloidectomy the patient’s neck and ear pain has resolved, although she continues to report occasional headaches and currently sees Neurology for management.
| |
|
Figure 3.
Computed tomography (sagittal cut) of the head and neck demonstrating elongation of the styloid process characteristic in stylohyoid or Eagle syndrome.
 |
|
|
Figure 4.
OCT of the RNFL 10 months after initial presentation demonstrating progressive thinning of the nerve fiber layer in the left eye. The average retinal nerve fiber layer thickness was 83 ?m for the right eye (A) and 73 ?m for the left eye (B).
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in