|
|
 |
 |
 |
 |
|
|
A 47-year-old man with a necrotic wound after trauma
Digital Journal of Ophthalmology 2021
Volume 27, Number 2
May 17, 2021
|
Printer Friendly
Download PDF |
|
|



Donald C. Hubbard II, BS | Texas A&M College of Medicine Jacob W. Fleenor, MD | Baylor Scott and White Eye Institute and Texas A&M College of Medicine Maxwell G. Su, MD | Baylor Scott and White Eye Institute and Texas A&M College of Medicine Jonathan H. Tsai, MD | Baylor Scott and White Eye Institute and Texas A&M College of Medicine
|
|
|
| Treatment | The patient underwent urgent right-sided orbital exenteration by our oculoplastics service, at which time the exenteration specimen was submitted for permanent sections. The plastic surgery service was consulted to aid with further surgical debridement of necrotic tissue extending beyond the orbit, which was performed serially over the next several days. The patient ultimately required a total of 6 separate debridement procedures.
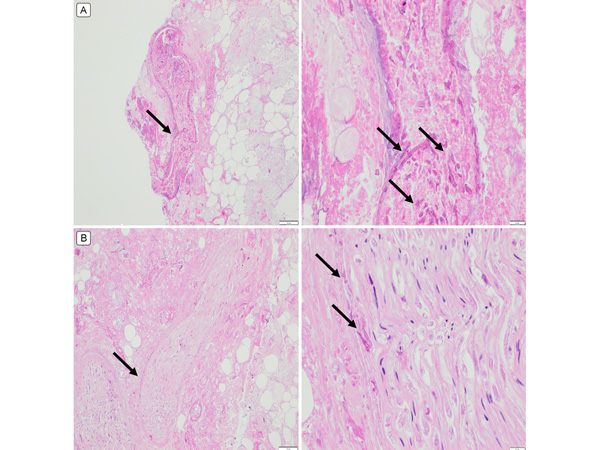
Surgical pathology consistently revealed angioinvasive mucormycosis in all specimens. There were also areas of intraneural invasion (Figure 5). This result was confirmed on staining with periodic acid-Schiff and Grocott-Gomori methenamine silver. No organisms were ever grown in culture.
He was started on liposomal amphotericin B, isavuconazole, and micafungin. The dressing placed over the wound was also soaked in amphotericin B and replaced several times throughout the day. After adequate surgical debridement, the patient’s exenteration site was clear of any visible eschar and began to granulate, showing optimistic signs of healing. Repeat CT imaging did not demonstrate any concern for evidence of further active fungal infection. On discharge, the patient completed 6 weeks of amphotericin B. He continued isavuconazole for a total of 8 months and had no recurrences of mucormycosis after discharge. The patient eventually received a skin graft and was fitted with a silicone prosthesis with an excellent aesthetic outcome.
| |
|
Figure 5.
A, Periodic acid Schiff (PAS) stain demonstrating angioinvasion of mucormycosis (arrows). The right panel demonstrates higher magnification of the area demarcated by the arrow in the left panel. B, PAS stain of the optic nerve showing focal areas of necrosis with invasive mucormycosis (black). Right panels, original magnification ×40; left panels, ×400.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in