|
|
 |
 |
 |
 |
|
|
A 24-year-old woman with sudden-onset, unilateral vision loss
Digital Journal of Ophthalmology 2019
Volume 25, Number 4
November 17, 2019
DOI: 10.5693/djo.03.2019.09.004
|
Printer Friendly
Download PDF |
|
|



Parisa Khalili | Al Zahra Eye Hospital, Zahedan University of Medical Sciences, Zahedan, Iran; Nazanin Ebrahimi Adib | Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran Hassan Khojasteh Jafari | Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran Reza Shamsi | Al Zahra Eye Hospital, Zahedan University of Medical Sciences, Zahedan, Iran; Shima Dehghani | Al Zahra Eye Hospital, Zahedan University of Medical Sciences, Zahedan, Iran
|
|
|
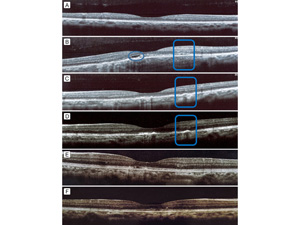
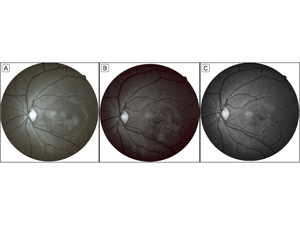
| Ancillary Testing | Initial diagnostic tests were performed on the 10th day of disease onset. Optical coherence tomography (OCT) revealed a dome-shaped deposition of hypo- and hyper-reflective material in an area beneath the fovea, with disruption of the inner segment–outer segment (IS/OS) junction and anterior dislocation of retinal layers. Additionally, compared to the normal-appearing right eye (Figure 2A), there was choroidal thickening and loss of the normal pattern of the choriocapillaris lumen (Figure 2B). Red-free images showed a hyper-reflective patch corresponding to the lesion seen on fundus examination (Figure 3A).
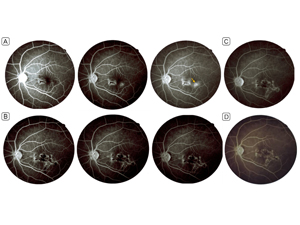
Fluorescein angiography (FA) 10 days after disease onset revealed a hypofluorescent patch with hyperfluorescent margins (1/2 disc diameters), smaller than the funduscopic lesion, along with a small nodule of adjacent hyperfluorescence corresponding to leakage (1/4 disc diameters). The margins of the lesion showed leakage and staining in the late phases of the angiogram (Figure 4A).
Testing also included a purified protein derivative (PPD) skin test due to the serpiginoid pattern of the lesion, the leakage observed on FA, and tuberculosis being endemic in the region. The patient had a positive PPD test (15 mm of induration). | |
|
Figure 2
Optical coherence tomography. Ten days after disease onset of the disease the right eye (A) appeared normal; the left eye (B) had dome-shaped heterogeneous hyper-reflective depositions in the outer retina, beneath the fovea, with disruption of the outer retinal layers, and a hyporeflective area (blue circle) attributable to fluid and hyper-reflectivity of the outer nuclear layer temporal to the fovea. In the 4th (C) and 7th (D) weeks of follow-up the undulations and irregularities in the retinal pigment epithelium layer (RPE) became less visible; the hyper-reflective depositions and fluid largely subsided. The junction of the inner and out segments seemed to reappear in the 7th week. In the 10th month (E) the outer retina appeared partially restored, and the nodular areas of thickened RPE were resolving. In the 19th month (F) the outer retinal abnormalities largely resolved.
 |
|
|
Figure 3
Red-free imaging. A nonhomogenous hyper-reflective patch was seen in the 1st (A) and 4th (B) week of follow-up. The margins became sharper and better demarcated, and the center appeared more hypo-reflective in the 4th week. In the 10th month of follow-up (C), the lesion became smaller and borders better delineated. The number and intensity of central hypo-reflective areas increased and led to a more distinct honey-comb pattern.
 |
|
|
Figure 4
Fluorescein angiography. Ten days after disease onset, early- to late-phase images (A) show a macular hypofluorescent patch, with hyperfluorescent margins and leakage in late phases and a small nearby leaking nodule (yellow arrow). In the 4th week of follow-up, the early- to late-phase images (B) show the leaking nodule merged with the rest of the lesion, acquiring a serpiginous morphology. In the 7th week (C), no leakage is evident; no change was observed in the size or the angiographic pattern from the 4th week, and the lesion evolved into a honey-comb pattern. At 19 months’ follow-up (D) the lesion appears stable, with no significant change in size/pattern or signs of reactivation.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in