|
|
 |
 |
 |
 |
|
|
A 24-year-old contact lens wearer with unilateral vision loss requiring penetrating keratoplasty
Digital Journal of Ophthalmology 2019
Volume 25, Number 2
June 30, 2019
DOI: 10.5693/djo.03.2019.06.001
|
Printer Friendly
Download PDF |
|
|


 Jonathan T. L. Lee, MBBS, BMedSc
Jonathan T. L. Lee, MBBS, BMedSc | Department of Ophthalmology, Alfred Health, Melbourne, Victoria, Australia Chengde Pham, MBBS, BMedSci | Department of Ophthalmology, Alfred Health, Melbourne, Victoria, Australia Edward Greenrod, MBBS, FRANZCO | Department of Ophthalmology, Alfred Health, Melbourne, Victoria, Australia
|
|
|
| Treatment | On suspicion of a fungal infection, the patient was admitted for hourly topical cefazolin 5%, tobramycin 0.3%, and voriconazole 1% drops. Initial corneal scrapings did not elicit microbial growth at 8 days. A corneal biopsy was performed, and filamentous fungal elements were identified. Intrastromal voriconazole (50 μg/0.1 mL) was injected circumferentially around the edge of the infiltrate to midcorneal depth, and twice daily oral voriconazole 200 mg and hourly topical natamycin 5% were introduced to replace the antibiotics.
Seven days following admission, visual acuity in the left eye deteriorated to counting fingers. Examination revealed a 2.0 × 2.0 mm corneal perforation. A 4.0 mm Tenon’s capsule patch graft was applied under general anesthesia. Three days postoperatively, visual acuity remained unchanged, and there was interval development of 4+ anterior chamber inflammation and a small hypopyon. Anterior chamber paracentesis was performed, with injections of intracameral and intrastromal voriconazole (50 μg/0.1 mL) as well as intracameral amphotericin B (5 μg/0.1 mL). Oral voriconazole was increased to 300 mg twice daily after consultation with the Infectious Diseases unit.
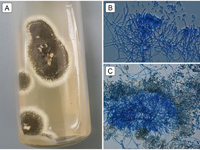
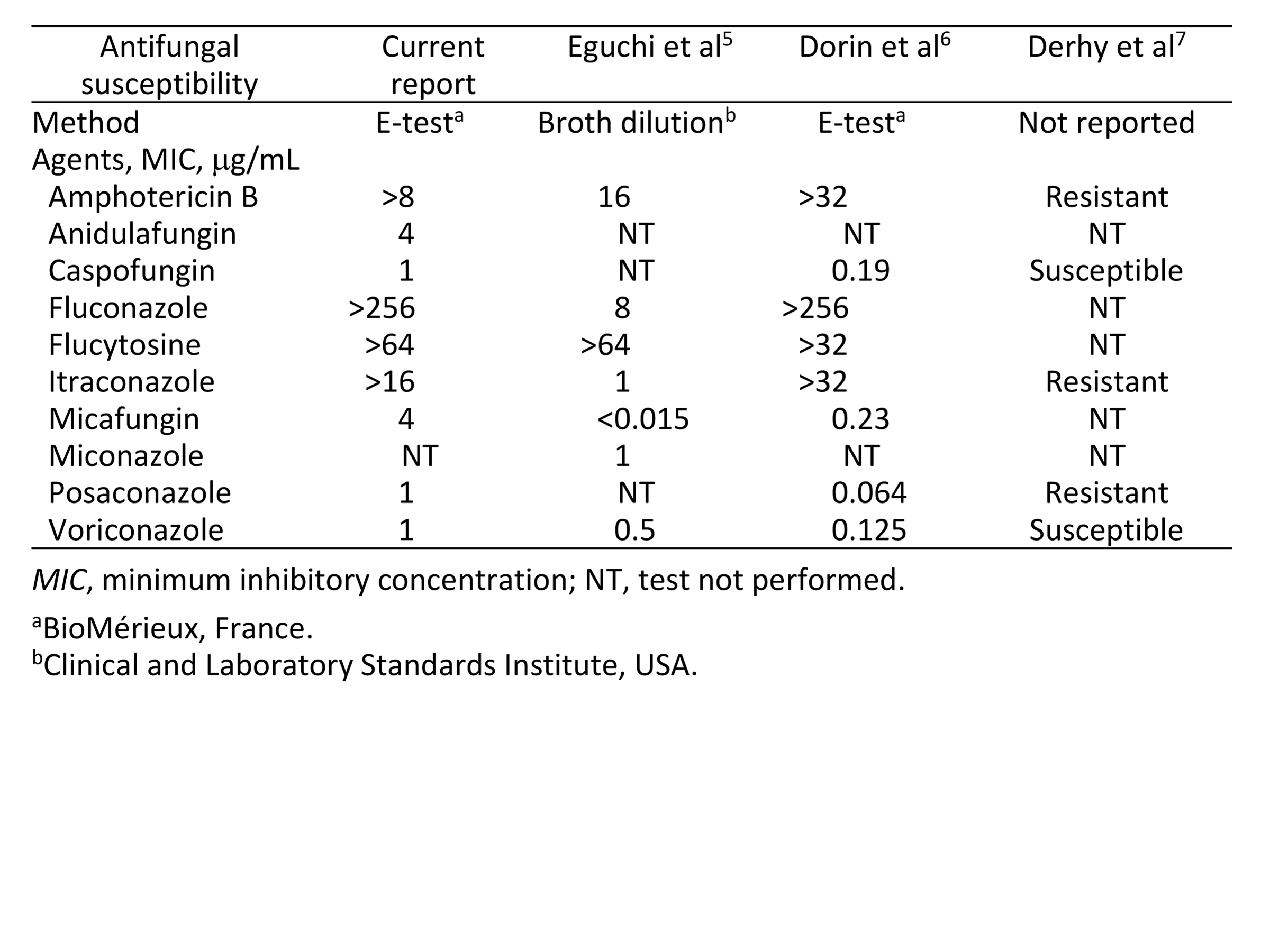
Isolates from the corneal biopsy grew olivaceous green colonies consistent with Metarhizium anisopliae after 10 days at 25° C on potato dextrose agar (Figure 2). Minimum inhibitory concentrations of several antifungal drugs were determined (Table 1).
Seventeen days following admission, the corneal glue patch dislodged. A 5.5 mm peripheral therapeutic penetrating keratoplasty was performed, with repeat intracameral, intrastromal, and subconjunctival voriconazole injections (50 μg/0.1 mL). A small iridectomy was performed where iris tissue was adherent to the perforation site.
Postoperative assessments were satisfactory with a clear graft and quiet anterior chamber. On discharge, the patient was commenced on topical cyclosporine A 1% drops 4 times daily and continued on her regular dose of topical and systemic voriconazole. The eye remained quiet; hence, topical dexamethasone 0.1% drops 4 times a day was introduced on day eleven post-keratoplasty for prevention of rejection. A 5-week course of oral voriconazole was completed, and topical voriconazole was gradually weaned over 9 weeks (Figure 1B). Fifteen months after keratoplasty best-corrected visual acuity in the left eye was 20/20, with refraction of −3.50 −1.00 ×60, with no evidence of infective recurrence or graft rejection. | |
|
Figure 2
Metarhizium anisopliae strain isolated in the present case. A, Olivaceous-green colonies grown on potato dextrose agar at 25° C for 10 days. B, Specialized fungal stalks (conidiophores) aggregated in dense tufts with verticillate branching. C, Yellow-green cylindrical-shaped fungal spores (conidia), produced in long chains on conidiophores.
 |
|
|
Table 1
Antifungal minimum inhibitory concentrations for ophthalmic isolates of Metarhizium anisopliae
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in