|
|
 |
 |
 |
 |
|
|
A 45-year-old man with unilateral optic disc edema and vision loss
Digital Journal of Ophthalmology 2019
Volume 25, Number 1
March 29, 2019
DOI: 10.5693/djo.03.2019.02.002
|
Printer Friendly
Download PDF |
|
|


 Benjamin G. Jastrzembski, MD
Benjamin G. Jastrzembski, MD | Division of Ophthalmology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts; Department of Ophthalmology, Hospital for Sick Children, University of Toronto, Toronto, Ontario Nurhan Torun, MD | Division of Ophthalmology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts
|
|
|
| Treatment | Steroid treatment was initially deferred because of concern for an infectious etiology. Eleven days after presentation, the patient’s visual acuity had declined to 20/400 in the left eye, and the infectious work-up was negative. At that time, the patient was started on prednisone 80 mg daily.
Thirty-three days following the initiation of steroids visual acuity improved to 20/30 in the left eye. MRI of the orbit with and without contrast performed at that time showed near resolution of the enhancement (Figure 4); 53 days following the initiation of steroids showed the disc edema and macular star in the left eye had resolved (Figure 5).
With taper of prednisone to 10 mg over the next 3 months, the patient’s visual acuity in the left eye declined to 20/40, requiring an increase in the steroid dose.
The patient was placed on monthly pulse intravenous cyclophosphamide for 3 months followed by oral daily azathioprine. Despite this immunomodulatory therapy, the patient was unable to be weaned from steroid therapy over the 2 years following initial presentation. At prednisone doses below 10 mg, he reported decreased vision in the left eye and demonstrated left optic nerve sheath enhancement on MRI. His condition remained exquisitely sensitive to steroids, with an increase in prednisone consistently effective in resolving his symptoms and MRI findings. The patient was switched to adalimumab, which facilitated discontinuation of corticosteroids. At his most recent visit, 6 months following initiation of adalimumab, the patient’s visual acuity was stable (20/25 in each eye), and the examination showed temporal pallor of the left optic nerve. Humphrey 30-2 SITA-Fast automated visual field showed a corresponding nasal defect in the visual field of the left eye (Figure 6). | |
|
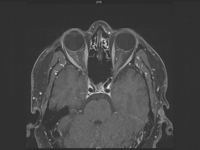
Figure 4
T1-weighted, post-contrast axial MRI of the orbit showing interval improvement in enhancement of the left optic nerve sheath complex.
 |
|
|
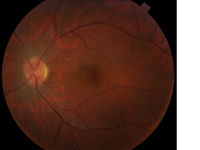
Figure 5
Fundus photograph of the left eye showing resolution in disc edema and macular star, with residual exudates in the nasal macula.
 |
|
|
Figure 6
Final Humphrey 30-2 SITA-fast automated visual field testing with nasal defect in the left eye.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in