|
|
 |
 |
 |
 |
|
|
A 45-year-old man with unilateral optic disc edema and vision loss
Digital Journal of Ophthalmology 2019
Volume 25, Number 1
March 29, 2019
DOI: 10.5693/djo.03.2019.02.002
|
Printer Friendly
Download PDF |
|
|


 Benjamin G. Jastrzembski, MD
Benjamin G. Jastrzembski, MD | Division of Ophthalmology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts; Department of Ophthalmology, Hospital for Sick Children, University of Toronto, Toronto, Ontario Nurhan Torun, MD | Division of Ophthalmology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts
|
|
|
| Diagnosis and Discussion | The patient was a 45-year-old man with gradual, painless decrease in vision in the left eye presenting with unilateral optic disc edema, partial macular star, and tram track enhancement of the left optic nerve sheath on MRI. He was diagnosed with idiopathic optic perineuritis and was treated successfully with corticosteroids and later adalimumab.
Two reports in the literature have presented similar cases of idiopathic optic perineuritis with unilateral disc edema and a macular star.(14,15) Zhang et al reported a case involving enucleation because of pain and a concern for an optic nerve sheath meningioma; pathology demonstrated idiopathic optic perineuritis.(14) Wals et al. described a patient with a macular star, disc edema, and optic perineuritis who improved without treatment to baseline vision in 11 months; they presented the case as simultaneous optic perineuritis and neuroretinitis.(15) In the case described here, the partial macular star is incomplete and indicates secondary subretinal fluid and exudation from the primary inflammation of the optic disc and optic sheath. For the present case, the diagnosis of optic perineuritis with associated optic disc and macular edema is more appropriate than simultaneous optic perineurits and neuroretinitis.
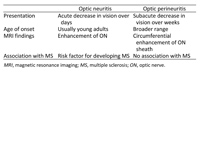
This case highlights the importance of differentiating between optic neuritis and optic perineuritis, which is relevant clinically because of the similarity of presentation and difference in treatment (Table 1). Optic perineuritis and optic neuritis may be confused because patients with both diseases present with painful, monocular vision loss and disc edema. However, vision loss in optic perineuritis progresses over weeks, whereas in optic neuritis vision typically declines over the course of a few days. Long-term optic neuritis is associated with a 50% 15-year risk of developing multiple sclerosis (MS), while there is no known relationship between optic perineuritis and MS (7,16). Finally, MRI is crucial to differentiate the diseases. MRI primarily shows enhancement of the optic nerve itself in optic neuritis and in the nerve sheath in optic perineuritis.(7) | |
|
Table 1
Table 1. Differentiating optic neuritis and optic perineuritis(6)
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in