|
|
 |
 |
 |
 |
|
|
A 15-year-old-boy with an optic neuropathy
Digital Journal of Ophthalmology 2017
Volume 23, Number 4
December 5, 2017
DOI: 10.5693/djo.03.2015.06.001
|
Printer Friendly
Download PDF |
|
|



David B. Lazar, MD | Department of Ophthalmology, Louisiana State University, New Orleans, Louisiana Adham B. Hariri, MD | Department of Ophthalmology, Ochsner Clinic Foundation, New Orleans, Louisiana
|
|
|
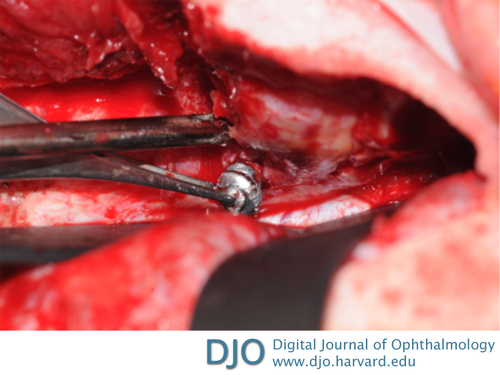
| Treatment | Oral steroids were restarted to decrease the orbital edema and treat his compressive optic neuropathy. A transcranial orbitotomy with a cranio-orbital approach was performed for exploration and removal of the foreign body. Removal of the orbital roof allowed for total exposure of the posterior aspect of the superior orbit, including the apex on the left side. An intraoperative navigation system was used to confirm the exact location of the pellet within the orbital apex. An incision through the periorbita was performed and extended to expose the entire pellet (Figure 3). A 5 mm foreign body was removed and further exploration revealed residual small foreign body pieces, which were removed and followed by copious irrigation of the field. Exploration of the inner aspect of the temporalis muscle revealed the site of entry and damaged tissue. Neurosurgery completed the procedure by closing the craniotomy. All metallic pieces and removed tissue were sent to pathology for documentation.
Postoperatively, the patient was admitted to the pediatric neuro-critical care unit. Repeat CT scan showed no evidence of acute intracranial hemorrhage or sulcal effacement. On postoperative day 1, there was complete resolution of the left afferent pupillary defect, and the patient’s visual acuity returned to 20/20 in the left eye. The patient was discharged on postoperative day 4 with resolution of eye pain and no restriction in his extraocular movements. He was followed closely for 3 months, with no further complications.
| |
|
Figure 3
Intraoperative photograph showing the reflected left frontal lobe of the brain and demonstrating the extraction of the pellet lodged in the posterior apex of the left orbit, through the removed orbital roof and incised periorbita.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in