|
|
 |
 |
 |
 |
|
|
30 year old man with painless, slowly progressive, bilateral visual loss
Digital Journal of Ophthalmology 1996
Volume 2, Number 9
December 10, 1996
|
Printer Friendly
|
|
|
|
|
|
|
| Diagnosis and Discussion | Terrien's Marginal Degeneration
Clinical Course:
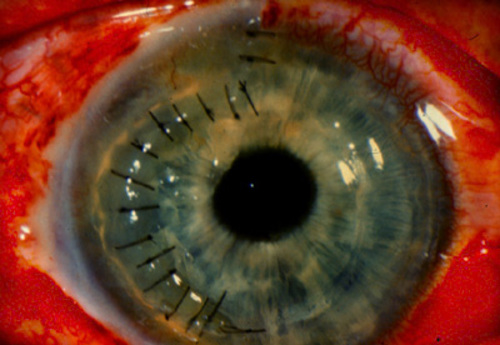
From the slit lamp appearance this patient was diagnosed with Terrien's marginal degeneration. Because the patient had a high degree of with-the-rule astigmatism, rigid gas-permeable contact lenses were prescribed. In the left eye the rgp contact lens was tolerated and gave the patient 20/20 vision. However, in the right eye the best corrected vision was 20/200 and the patient could not tolerate the contact lens. He continued to be managed conservatively, until on one subsequent follow up visit, an area of a descemetocele was noted at a 10:30 position in the right eye. For this reason, the decision was made to proceed with a partial thickness crescentic corneal patch graft (Figure 3.)
Terrien's marginal degeneration is a rare peripheral corneal stromal disorder of unknown origin. It presents as painless, blurred vision due to high astigmatism which is usually against-the-rule or oblique. The eye is usually quiet without any signs of inflammation. The tissue changes are slowly progressive and often bilateral but usually asymmetric. It is more prevalent in men.
The most common area involved is the superior limbus. The initial manifestation is described as fine, yellow-white perilimbal punctate stromal opacifications. This is followed by superficial peripheral corneal neovascularization and leads to thinning parallel to the limbus. Lipid deposition may develop along the anterior lip, which is steeply sloped, in contrast to the posterior lip which slopes gradually. Over several years, progressive circumferential thinning may occur, and even trivial trauma can cause a rupture of the ectatic cornea. Spontaneous perforations occur in up to 15 % of cases.
Histopathologic examination reveals an intact epithelium, loss of Bowman's membrane, and sometimes superficial stroma. Descemet's membrane is usually intact, thickened or thinned. Histiocytes with a high degree of lysosomal activity are responsible for destruction of collagen fibrils.
Histopathologic examination reveals an intact epithelium, loss of Bowman's membrane, and sometimes superficial stroma. Descemet's membrane is usually intact, thickened or thinned. Histiocytes with a high degree of lysosomal activity are responsible for destruction of collagen fibrils.
Treatment is based on both the visual symptoms and the biomicroscopic findings. It consists initially of observation, treating the induced astigmatism as well as possible using spectacles, followed by a trial of rigid gas-permeable contact lenses when spectacles are unsatisfactory. Most patients can achieve adequate visual function with one of these options. In severe cases where the integrity of the eye is threatened, surgical intervention can be offered. Several procedures are currently performed: simple primary surgical REPAIR of ectatic area, sclero-corneal autotransplantation, corneo- scleral lamellar keratoplasty, and annular keratoplasty. | |
|
Figure 3
Slit lamp photo one day post lamellar crescentic keratoplasty
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in