|
|
 |
 |
 |
 |
|
|
49 year old man with 6 months of swelling around the right eye
Digital Journal of Ophthalmology 1998
Volume 4, Number 20
July 6, 1998
|
Printer Friendly
|
|
|
|
|
|
|
| Diagnosis and Discussion | Posterior Scleritis with Choroidal Detachment and Angle Closure Glaucoma
This case represents an atypical cause of a narrow anterior chamber angle and elevated intraocular pressure. Unilateral narrow angle should raise questions as to secondary causes of shallowing the anterior chamber. The possibilities include annular ciliochoroidal detachment, phakomorphogenic, and a posterior intraocular mass.
Annular ciliochoroidal detachment causing secondary angle closure is well documented. The detachment creates an anterior rotation of the ciliary body on the scleral spur. The resultant angle closure leads to an elevated intraocular pressure. Annular ciliochoroidal detachments are caused by posterior scleritis, ciliary body ring melanoma, intraocular surgery, and Uveal Effusion Syndrome. Ultrasonography, both B-scan and UBM, are crucial in identifying the cause.
The differential diagnosis of choroidal detachment is extensive. There are iatrogenic causes (medications-HCTZ/triamterene, post operative, PRP, RD repair), inflammatory causes (Scleritis, orbital pseudotumor, VKH, Wegener's, etc.), vascular causes (C-C fistula, dural-sinus fistula, eclampsia, Valsalva), malignant causes (metastasis, leukemia, multiple myeloma), and anatomical causes (nanophthalmos, Uveal effusion syndrome). The clinical history will often lead to the diagnosis. If the etiology is unclear, ancillary testing is warranted.
On ultrasonography, the classic finding in choroidal detachment is the abrupt elevation of the detached choroid. The choroidal signal is thicker than that of detached retina and the choroidal detachment will not undulate with eye movements as a rhegmatogenous retinal detachment would.
The reported case shows a classic choroidal detachment. (Figure) Ultrasonography also revealed a thickened sclera with fluid in sub-Tenon's space. These findings are characteristic of posterior scleritis. Ultrasound is the preferred diagnostic modality for posterior scleritis. The CT scan, which some feel is as effective as ultrasound in diagnosis, showed thickened sclera and a prominent choroidal detachment.
Posterior scleritis is a disease that can present with an isolated choroidal mass, choroidal effusion, choroidal folds, cystoid macular edema, and exudative macular detachment in a patient with ocular pain. It can be bilateral and affects women more often than men. The most common cause is Rheumatoid arthritis, which accounts for nearly 30% of cases. Less common causes include Wegener's granulomatosis, orbital inflammatory pseudotumor, VKH, and sympathetic ophthalmia. The diagnosis of posterior scleritis is often delayed due to its nonspecific presentation. Non-steroidal anti- inflammatory agents have been used to successfully treat posterior scleritis, however, traditionally, steroids are needed. Both periocular and systemic steroids have been reported to be effective. A work-up is indicated in those cases that are bilateral.
KEY POINTS:
- Always perform goinioscopy on both eyes in the setting of angle closure.
- If the clinical picture does not concur with the presumed diagnosis, one must rethink the diagnosis.
- Annular ciliochoroidal detachments can cause secondary angle closure due to anterior rotation of the ciliary body on the scleral spur. | |
|
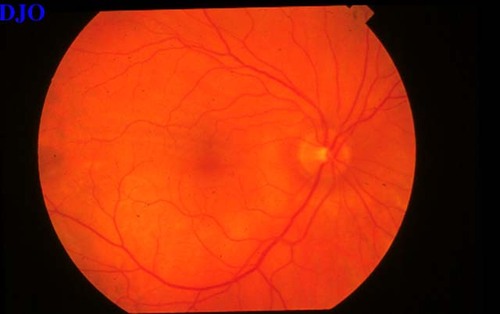
Figure 6
Two weeks post-treatment with naproxen. The choroidal detachments have nearly resolved. Subtle choroidal folds are noted superior to the fovea
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in