|
|
 |
 |
 |
 |
|
|
A 50-year-old man with a long-standing, large-angle exotropia and limitation of adduction in the left eye
Digital Journal of Ophthalmology 2013
Volume 19, Number 4
December 30, 2013
DOI: 10.5693/djo.03.2013.09.004
|
Printer Friendly
Download PDF |
|
|



Reshma A. Mehendale, MD | Department of Ophthalmology, Boston Children’s Hospital, and Harvard Medical School, Boston, Massachusetts Anat O. Stemmer-Rachamimov, MD | Department of Pathology, Massachusetts General Hospital, and Ophthalmic Pathology, Massachusetts Eye and Ear Infirmary, and Harvard Medical School Linda R. Dagi, MD | Department of Ophthalmology, Boston Children’s Hospital, and Harvard Medical School, Boston, Massachusetts
|
|
|
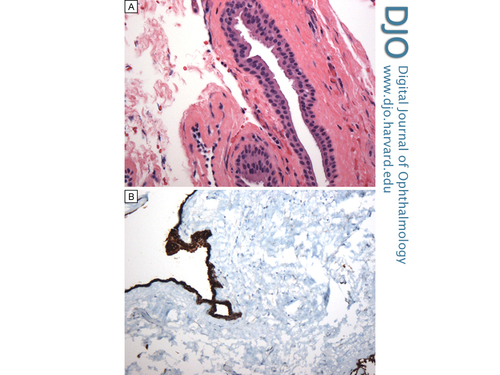
| Diagnosis and Discussion | Histopathological examination of the excised lesion showed a cystic structure with a thin wall lined by a double layer of non-keratinizing cuboidal epithelium. The cyst content was acellular, proteinaceous material. No skin appendages or goblet cells were identified, and the epithelial cells did not have cilia. In some areas the cells appeared to have luminal projections, suggestive of apical apocrine snouts (Figure 3A). Immunohistochemistry for pan keratin highlighted the epithelial lining (Figure 3B). Immunostaining performed to identify apocrine differentiation was negative, and epithelial cells were immuno-negative for gross cystic disease fluid protein-15. Actin immunostaining was negative for actin positive myoepithelial cells.
The lining of the cyst in the present case was composed of epithelial cells, and this limited the differential to epidermal cyst, conjunctival cyst, respiratory epithelial cyst, and apocrine gland cyst. The lack of keratin production and of squamous differentiation excluded the possibility of epidermal cyst. The lack of cilia and goblet cells made respiratory epithelial cyst unlikely reducing the differential to an apocrine gland cyst (sudoriferous cyst) or a conjunctival cyst. Apocrine gland cysts, which may (rarely) occur in the anterior portion of the orbit, are congenital in nature and thought to develop from entrapped epithelial cells destined to form the glands of Moll. Most conjunctival cysts develop secondary to implantation following ocular trauma or surgery. A primary, congenital form has been described that arises along the common sheath of the superior rectus muscle and levator palpebrae superioris muscle that is thought to result from misdirected cleavage of mesoderm.(2)
Development of a clinically significant giant conjunctival cyst as a complication of strabismus surgery has been reported, albeit rarely.(3-6) This complication has a reported incidence of 0.25% after strabismus procedures.(7) The purple/blue grayish hue of such cysts, noted in our patient, has been previously cited along with the frequent delay in growth, secondary strabismus, and clinical presentation for evaluation.(6,8)
Although thermal cauterization or intralesional injection with isopropyl alcohol have been successfully used to shrink some conjunctival cysts,(9,10) these techniques do not address the large secondary incommitant strabismus associated with many giant conjunctival cysts. Management by marsupialization of the cyst has been reported to correct a simple epithelial cyst adjacent to a muscle.(11) In cases such as the present one, where the cyst has encapsulated muscle fibers and is associated with strabismus, careful surgical excision remains the mainstay of therapy because it allows salvaging the healthy rectus muscle and recreating a new attachment to the globe.(6,8,9)
When examining a patient with an orbital mass with or without associated strabismus, it is vital to take into account the history of previous ocular surgery or trauma and to consider the possibility of a giant conjunctival cyst. The use of imaging modalities, such as orbital MRI or ultrasound, can help provide useful information regarding the consistency of the mass and its relationship to adjacent structures. An isolated cyst without adjacent bony erosion or soft tissue invasion is likely to be benign histologically, although it is not benign if it causes secondary strabismus, displacement, or compression of surrounding structures. Imaging in the present case provided invaluable insight into the cystic structure of the mass, and the extreme displacement of the medial rectus insertion; understanding this anatomical relationship prevented inadvertent loss of the medial rectus at the time of repair. Histopathological examination confirmed the nature of the lesion in this case, reassuring patient and surgeon alike. | |
|
Figure 4
Histological characteristics of the mass. A, Hematoxylin and eosin stain showing a thin wall lined by a double layer of non-keratinizing cuboidal epithelium; there are no identifiable goblet cells (original magnification × 40). B, Immunohistochemistry for pan keratin highlighting the epithelial lining (original magnification × 20).
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in