|
|
 |
 |
 |
 |
|
|
A 48-year-old woman with redness, photophobia, and eye discomfort
Digital Journal of Ophthalmology 2013
Volume 19, Number 2
May 1, 2013
DOI: 10.5693/djo.03.2013.01.003
|
Printer Friendly
Download PDF |
|
|


 Benjamin Erickson, MD
Benjamin Erickson, MD | Bascom Palmer Eye Institute, Miami, Florida Aleksandra Rachitskaya, MD | Bascom Palmer Eye Institute, Miami, Florida Thomas Shane, MD | Bascom Palmer Eye Institute, Miami, Florida
|
|
|
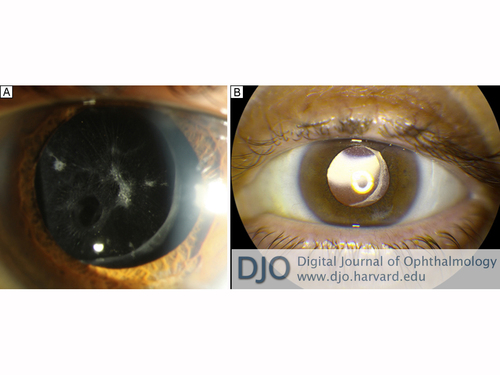
| Diagnosis and Discussion | Once the inflammation quieted further, phacoemulsification with posterior chamber intraocular lens placement was performed. After cortical cleanup, an oval-shaped hole was observed in the posterior lens capsule, corresponding with unrecognized trauma sustained during vitrectomy (Figure 2). This finding supported the presumed clinical diagnosis of phacoantigenic endophthalmitis. The patient’s inflammation subsided and her IOP normalized without the need for additional glaucoma drops or for steroids beyond the typical post-cataract extraction course. Unfortunately, the patient developed an occult macular hole, and this limited her final central visual acuity. She pursued further evaluation with the retina service, but has not undergone further surgical intervention to date.
Phacoantigenic endophthalmitis is a rare granulomatous uveitis caused by altered immune tolerance to lens proteins following capsular disruption. The traditional term, “phacoanaphylactic endophthalmitis,” is misleading because inflammation results from immune complex formation rather than IgE crosslinking and histamine release. When first described by Straub in 1919, basic immunologic mechanisms were not yet understood, and “anaphylaxis” was used to describe all sudden-onset inflammation.(2,3)
Until the 1980s, it was erroneously believed that the immune system attacked antigens previously sequestered by the lens capsule. Lens-related antigens have since been identified in organs throughout the body and lens proteins are known to be present in low concentrations in the aqueous of normal individuals.(4) There are many cases in which the lens capsule is disrupted without inciting inflammation. Disruption is therefore necessary but not alone sufficient to cause an immunologic response. The exact stimulus for alloimmunization remains unclear, but the process of immune complex formation and inflammatory cell recruitment has been well elucidated.(5)
Ultrasound findings consistent with a fulminant infectious endophthalmitis include abundant vitreous debris, often in loculated pockets, inflammatory membranes, and occasionally retinal or choroidal detachment. While B-scans in early endophthalmitis may not demonstrate classical findings, this paucity would be unusual in a patient presenting within 10 days of symptoms.
Phacoantigenic endophthalmitis most often follows surgical or traumatic penetration of the lens capsule but also has been described after spontaneous capsular rupture resulting from advanced, swollen cataracts. Inflammation often develops within days to weeks of the inciting event, but latency periods of up to 59 years have been reported.(4) Peak incidence is in the fifth to seventh decades despite higher rates of ocular trauma in younger individuals.(2,4)
Though rare, phacoantigenic endophthalmitis seems to be an under-recognized condition. In a series of 144 cases of histopathologically confirmed phacoantigenic endophthalmitis, Thatch et al found that the pre-enucleation diagnosis was correct in only 5% of cases.(2) Clinically, phacoantigenic endophthalmitis can be difficult to distinguish from other forms of postoperative uveitis. Patients often present with photophobia and ciliary reaction. Findings can range from mild anterior uveitis to fulminant endophthalmitis with hypopyon. Mutton fat keratic precipitates and peripheral anterior synechiae are characteristic but not universal. Most manifestations of phacoantigenic endophthalmitis are anterior, but late sequellae may include mononuclear choroiditis, optic atrophy, retinal perivasculitis, or retinal detachment.(4)
If clinical suspicion is high, early evaluation and treatment for infectious endophthalmitis is critical. Several recent studies report the utility of anterior chamber paracentesis for cytologic evaluation and/or western blot quantification of lens protein concentration, but these procedures are not standard clinical practice.(6,7) Histopathology is not practical or necessary in many cases, but when performed, it typically reveals a zonal granulomatous pattern with concentric rings of polymorphonuclear leukocytes, epithelioid and giant cells, and mononuclear cells.
In cases of granulomatous anterior uveitis associated with lens capsule disruption, patients are initially treated with steroids. When only small lens fragments are retained, as after phacoemulsification, inflammation may subside with medical management alone. When phacoantigenic endophthalmitis follows lens trauma, as with our patient, surgery is required for definitive treatment. | |
|
Figure 2
A, Oval hole in the inferonasal posterior capsule from unrecognized intraoperative vitrector trauma. B, Result after placement of posterior chamber intraocular lens.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in