|
|
 |
 |
 |
 |
|
|
A 53-year-old woman with a severe headache, bilateral eye pain, blurred vision, and photophobia
Digital Journal of Ophthalmology 2011
Volume 17, Number 3
August 28, 2011
DOI: 10.5693/djo.03.2011.05.002
|
Printer Friendly
Download PDF |
|
|


 Pedro Barros, MD
Pedro Barros, MD | Department of Ophthalmology, Hospital Pedro Hispano, Porto, Portugal Liliana Paris, MD | Department of Ophthalmology, Hospital Pedro Hispano, Porto, Portugal Joana Martins, MD | Department of Ophthalmology, Hospital Pedro Hispano, Porto, Portugal Paula Tenedorio, MD | Department of Ophthalmology, Hospital Pedro Hispano, Porto, Portugal
|
|
|
| Treatment | She was treated with intravenous mannitol (100 g in 500 ml), oral acetazolamide (500 mg), and topical brimonidine tartrate 0.2%, timolol maleate 0.5%, and prednisolone acetate 1% in both eyes. Ninety minutes after mannitol administration, the IOP was 31 mm Hg in the right eye and 33 mm Hg in the left eye. Four hours later she was discharged with a prescription for topical brimonidine tartrate 0.2% twice daily, timolol maleate 0.5% twice daily, and prednisolone acetate 1% four times daily in both eyes. She was experiencing no major discomfort. The IOP on discharge was 27 mm Hg in the right eye and 29 mm Hg in the left.
Four days later visual acuity had improved to 20/30 in both eyes. The IOP was 16 mm Hg in the right eye and 17 mm Hg in the left, and the anterior chambers were deeper, with gonioscopy showing angle structures bilaterally. B-scan and ultrasound biomicroscopy revealed improvement of the uveal effusions and ciliary body swelling, respectively (Figure 2). Nine days after the episode the visual acuity returned to 20/20 in both eyes, the IOP was 13 mm Hg in the right eye and 14 mm Hg in the left eye, and the uveal effusion and ciliary body swelling had resolved completely (Figures 3-4). | |
|
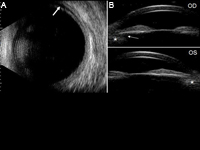
Figure 2
A, B-scan image 4 days after the episode shows improvement of uveal effusion. Choroidal effusion is still visible peripherally (arrow). B, Ultrasound biomicroscopy images 4 days after the episode show improvement of ciliary body edema (asterisk) mainly in the right eye (OD) with reappearance of the ciliary sulcus (arrow).
 |
|
|
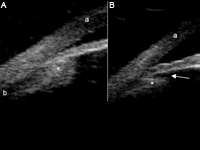
Figure 3
Ultrasound biomicroscopy images of angles and ciliary bodies 90 minutes after intravenous mannitol treatment (A) and 9 days after the episode (B). Corneal edema (a) disappeared as well as choroidal effusion (b) and ciliary body edema (asterisk) with backward rotation of the ciliary processes, reappearance of the ciliary sulcus (arrow), and consequent reopening of the anterior chamber angle.
 |
|
|
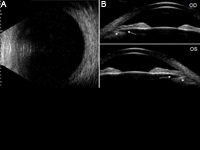
Figure 4
A, B-scan image 9 days after the episode shows complete resolution of choroidal effusion. B, Ultrasound biomicroscopy images 9 days after the episode show resolution of edema and anterior rotation of the ciliary body (asterisk) with good visualization of ciliary sulcus (arrows) in both eyes.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in