|
|
 |
 |
 |
 |
|
|
A 36-year-old man with a red eye
Digital Journal of Ophthalmology 2008
Volume 14, Number 9
April 13, 2008
|
Printer Friendly
|
|
|
|
|
|
|
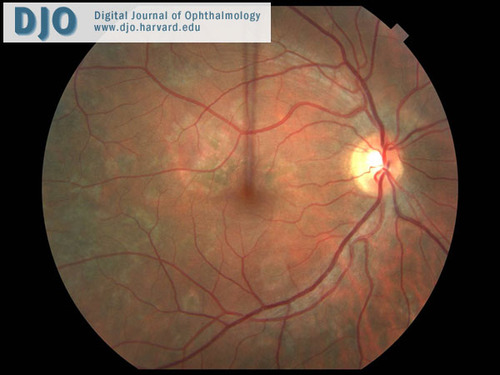
| Diagnosis and Discussion | Our patient was treated with immunosuppression for sympathetic ophthalmia and was closely monitored in the outpatient setting. His labs returned and excluded the other diseases in the differential. He developed nausea, anorexia, fatigue, and a mild rise in his blood pressure over the first week. He then developed periorbital pain around the left eye with a severe headache. He was admitted for a 3-day course of IV methylprednisolone. Rheumatology was consulted and the patient was switched from cyclosporine to mycophenolate mofetil. His symptoms and intraocular inflammation greatly improved. The choroidal lesions also improved (Figure 9). Oral prednisone and prednisolone drops were very slowly tapered and mycophenolate mofetil was gradually increased. Approximately 2 months later, the anterior chamber cells had finally cleared. At six months after initial presentation, the patient is currently on prednisone 12.5 mg and mycophenolate mofetil 1000 mg 2x/day. His right eye has remained quiet with subretinal scarring and 20/20 vision.
Sympathetic ophthalmia is a non-necrotizing, granulomatous panuveitis that generally spares the choriocapillaris.(2) The incidence is reported to be 0.2% after accidental trauma and less than 0.1% after surgical trauma.(3) It is theorized that sequestered intraocular antigens gain access to the lymphatic system after a penetrating ocular injury and the predominant cellular infiltrate has been found to be T lymphocytes.(4) Although sympathetic ophthalmia has been found to occur up to 66 years after injury, 65% of cases present between 2-8 weeks after injury and 90% of cases occur within 1 year.(2)
Patients often complain of vision loss, photophobia, and/or pain. Signs can include panuveitis, multifocal infiltrates at the level of the RPE or choroid, thickening of the uveal tract, optic nerve swelling, and/or exudative retinal detachment.
The diagnosis is one of exclusion but is suggested by bilateral uveitis after trauma or injury. Treatment initially consists of corticosteroids (topical, systemic, and/or periocular) and topical cycloplegics or mydriatics. When treated with steroids, the majority of patients retain 20/60 vision or better.(5) Given the long-term need for immunosuppression, a steroid-sparing agent becomes necessary to avoid the dangerous adverse effects of long-term steroid use. There is strong evidence that low-dose cyclosporine (a T-lymphocyte inhibitor) should be considered a first-line immunomodulator with or without concomitant low-dose corticosteroids in cases of chronic non-infectious uveitis (including sympathetic ophthalmia).(6) Mycophenolate mofetil is a newer immunomodulator with a better side effect profile. There is moderate evidence of efficacy showing that mycophenolate mofetil should be used for chronic non-infectious uveitis when other immunosuppressive drugs have failed or have not been tolerated.(7) Alkylating agents (i.e. chlorambucil or cyclophosphamide) and antimetabolites (i.e. azathioprine) or a combination of two immunosuppressive agents may also be considered in patients with resistant vision-threatening inflammation.(7) | |
|
Figure 9
A right eye fundus photo shows fading of the choroidal lesions after 2 weeks of treatment.
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in