A 71-year-old man with bilateral vision loss
Digital Journal of Ophthalmology 2017
Volume 23, Number 3
September 3, 2017
DOI: 10.5693/djo.03.2017.03.002
Volume 23, Number 3
September 3, 2017
DOI: 10.5693/djo.03.2017.03.002
Download PDF
The patient’s symptoms did not improve, and he was transferred to a tertiary care facility for additional workup. On further questioning, the patient endorsed new-onset headache of 2-3 weeks’ duration, severe pain with chewing, scalp pain, and weight loss. He denied recent eye or head trauma. He denied recent illness, fevers, chills, night sweats, cough, and shortness of breath. He denied recent alcohol or drug use, and he denied any history of sexually transmitted diseases.
Dilated fundus examination of the left eye was limited but showed 3+ optic nerve head edema. There was a cherry red spot. Arterioles were attenuated, and venules were dark and severely dilated (Figure 2). The peripheral retina was attached. There was no view posteriorly in the right eye.

Figure 1
Anterior segment photograph of the right eye demonstrating an edematous and opacified cornea without keratic precipitates.
Anterior segment photograph of the right eye demonstrating an edematous and opacified cornea without keratic precipitates.

Figure 2
Fundus photograph of the left eye demonstrating a cherry-red spot, attenuated arterioles, and dark, dilated venules.
Fundus photograph of the left eye demonstrating a cherry-red spot, attenuated arterioles, and dark, dilated venules.
Complete blood count was within normal limits with the exception of an elevated platelet count (484 ×103/mm3). Basic metabolic panel was remarkable for low sodium (132 mEq/L), potassium (2.3 mEq/L), chloride (95 mEq/L), and brain natriuretic peptide (6 mg/dL). Inflammatory markers were elevated: erythrocyte sedimentation rate (ESR) was 59 mm/hr, and C-reactive protein (CRP) was 7.53 mg/L (normal range, 0.02-0.7 mg/L). Additional testing that returned negative after diagnosis included purified protein derivative skin test, rapid plasma reagin, fluorescent treponemal antibody absorption test, anti-neutrophil cytoplasmic antibody (ANCA), and antinuclear antibody tests.
Maxillofacial computed tomography (CT) demonstrated no abnormalities. Magnetic resonance imaging (MRI) of the brain with and without contrast showed mild atrophy and chronic microvascular ischemic changes.
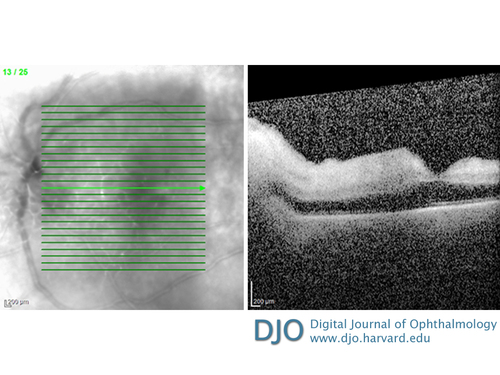
Figure 3
Optical coherence tomography (OCT) of the left eye revealed a diffusely thickened macula without fluid.
Optical coherence tomography (OCT) of the left eye revealed a diffusely thickened macula without fluid.
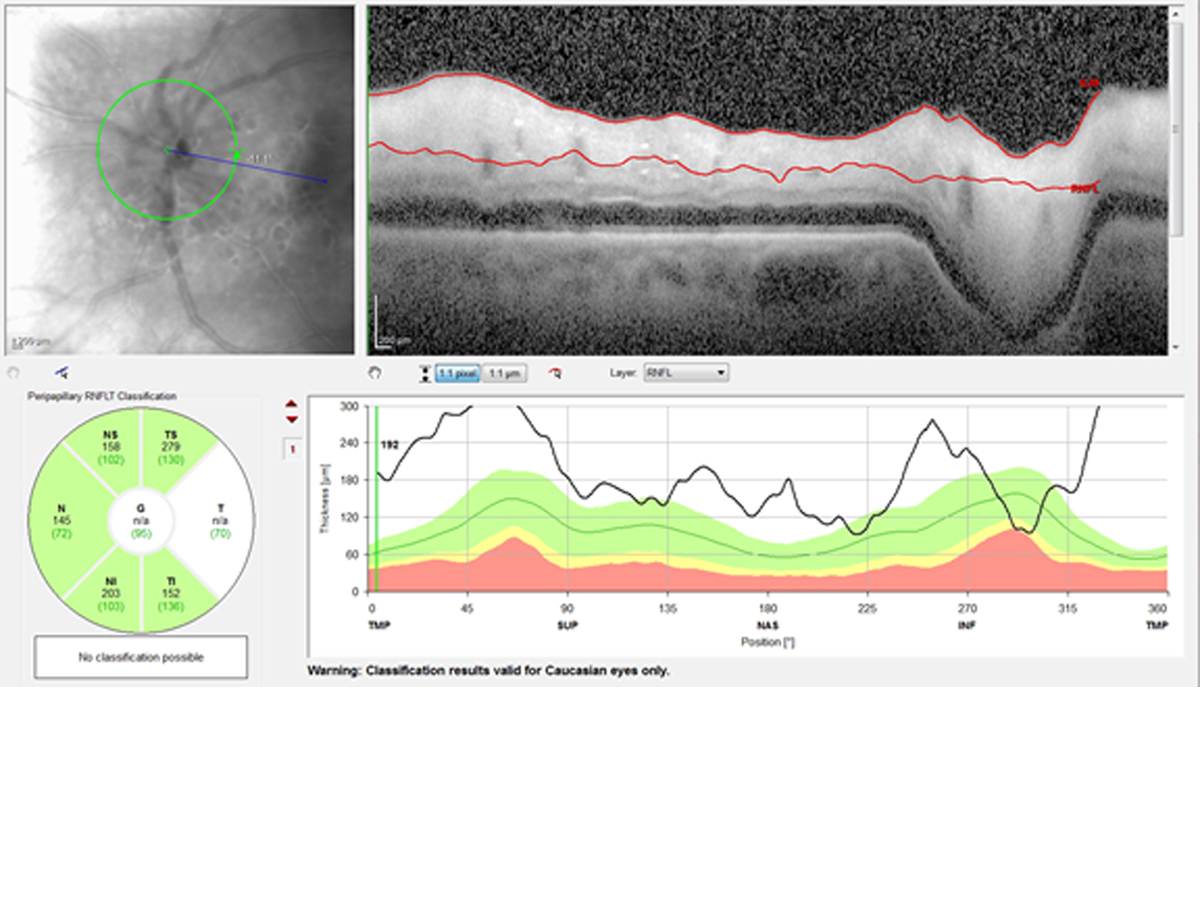
Figure 4
OCT retinal nerve fiber layer of the left eye showing thickening of the retinal nerve fiber layer around the disc suggesting optic nerve head edema.
OCT retinal nerve fiber layer of the left eye showing thickening of the retinal nerve fiber layer around the disc suggesting optic nerve head edema.
Although our patient was previously diagnosed with anterior uveitis, his clinical presentation, examination findings, and ancillary testing pointed to a vascular etiology of acute bilateral vision loss consistent with giant cell arteritis. In a patient >50 years of age, our history elicited several red flags, including severe new-onset headaches, jaw claudication, scalp tenderness, and recent unexplained weight loss.(2) In addition, his ESR and CRP were significantly elevated. Dilated examination of the left eye showed central retinal artery occlusion as well as involvement of posterior ciliary arteries with corneal opacification and hypotony due to anterior segment ischemia; together, the clinical picture favored occlusion of the ophthalmic artery.
It is important to consider the differential diagnosis for acute vision loss to no light perception, because there are few causes for such acute, profound vision loss. One must consider giant cell arteritis, other causes of ophthalmic artery occlusion, optic neuritis (neuromyelitis optica or multiple sclerosis), traumatic optic neuropathy, and nonorganic vision loss. In GCA, up to 21% of cases present with no light perception vision.(3) Although GCA oftentimes presents with evidence of optic disc or retinal ischemia on clinical examination, GCA can less commonly present with anterior segment ischemia,(4) posterior ischemic optic neuropathy, cranial nerve palsies, or Horner’s syndrome.
The visual prognosis of this patient presenting with no light perception in both eyes is poor, and he was lost to follow-up after hospital discharge. In a patient with unilateral or less severe vision loss due to GCA, appropriate and timely treatment may prevent a devastating visual outcome.
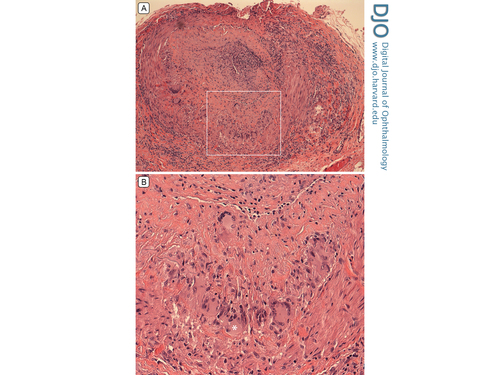
Figure 5
A, Histopathology (hematoxylin-eosin stain) of temporal artery biopsy showing “intense granulomatous arteritis,” with a nearly occluded artery lumen and inflammation in all vessel layers (original magnification ×10). B, Higher magnification of the segment delineated by the whited box shows multinucleated cells, one of which is indicated by the asterisk (original magnification ×25).
A, Histopathology (hematoxylin-eosin stain) of temporal artery biopsy showing “intense granulomatous arteritis,” with a nearly occluded artery lumen and inflammation in all vessel layers (original magnification ×10). B, Higher magnification of the segment delineated by the whited box shows multinucleated cells, one of which is indicated by the asterisk (original magnification ×25).
2. El-Dairi MA, Chang L, Proia AD, Cummings TJ, Stinnett SS, Bhatti MT. Diagnostic algorithm for patients with suspected giant cell arteritis. J Neuroophthalmol 2015;35:246-53.
3. Liu G, Glaser JS, Schatz NJ, Smith JL. Visual morbidity in giant cell arteritis: clinical characteristics and prognosis of vision. Ophthalmology 1994;101:1779-85.
4. McKillop E, Tejawani, D, Weir C, Jay J. Anterior segment ischaemia with giant cell arteritis. Can J Ophthalmol 2006;41:201-3.