A 35-year-old woman presenting with pain, reduced right-eye vision, and headache
Digital Journal of Ophthalmology 2015
Volume 21, Number 2
May 13, 2015
DOI: 10.5693/djo.03.2015.03.002
Volume 21, Number 2
May 13, 2015
DOI: 10.5693/djo.03.2015.03.002
Download PDF
For 2 years prior to this episode she complained of recurrent headaches every 2-4 months associated with similar visual aura. The headaches were not unilateral, and the visual symptoms were not limited to one side. She had been diagnosed with migraine in her teens; however, the headaches had now become more frequent, without change in nature. She described “flickering lights” that presented suddenly with reduced vision, “as if looking through a steamy window.” Each episode lasted 3-4 hours. She also noticed “rainbows” around bright lights, with “speckles, flashing lights, and blotches” in her vision. In the weeks before presentation, these attacks increased in frequency to almost daily, and sunlight was volunteered to be a trigger. There was no associated nausea, weakness, or other systemic symptoms. The ocular symptoms were now predominantly unilateral but similar to the symptoms that had been attributed to migraine in the past.
Previous assessments by ophthalmologists during the 2-year period prior to presentation found that her vision was stable, with deep anterior chambers. Vitreous was present up to the pupillary margin, but was not in the anterior chamber. The anterior hyaloid face was intact, intraocular pressures (IOPs) were normal, and the optic discs were healthy. No focal defects were detected on visual field testing. On one previous visit, when her IOP in the right eye was found to be elevated, vitreous was noted in the anterior chamber, although there was no evidence of iris bombe. The angles were open on gonioscopy, with scattered peripheral anterior synechiae in 90°-180° in the right eye, whereas the left eye had open angles in all quadrants, with no synechiae. The past intraocular surgery was considered the likely etiology for the peripheral anterior synechiae. During this period, a neurologist confirmed that these episodes were representative of migraine.
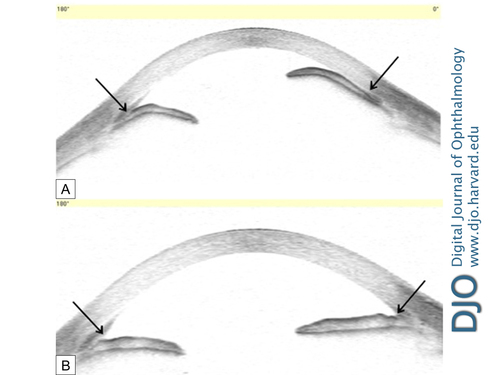
Figure 1
A, Anterior segment optical coherence topography of patient with pupillary-block glaucoma with elevated intraocular pressure showing anterior bowing of the iris and closure of the iridocorneal angle (arrows). B, After treatment, the anterior chamber has deepened with open angles and a flat iris contour (arrows).
A, Anterior segment optical coherence topography of patient with pupillary-block glaucoma with elevated intraocular pressure showing anterior bowing of the iris and closure of the iridocorneal angle (arrows). B, After treatment, the anterior chamber has deepened with open angles and a flat iris contour (arrows).
In this situation, Shaffer also describes the role of miotics in increasing the tension of the pupil causing a plugging effect on the vitreous thereby creating a resistance to aqueous outflow.(2) This may explain the reason for sunlight acting as a trigger for headaches in our patient, which were likely intermittent episodes of pupillary block.
An illustration from Hitching’s 1979 paper is remarkably similar to the findings documented on the day of the acute episode (Figure 2).(1) There have been several reports of intermittent-angle closure episodes (in phakic but not aphakic patients) misdiagnosed as migraine prior to arriving at the correct diagnosis. In these cases, there was an association with high hypermetropia or shallow anterior chambers, prompting ophthalmology referral. Assessment for angle width confirmed intermittent-angle closure.(3-5)
In aphakic pupillary block, the anterior chambers can be deep, except in an acute setting. Posner has described 3 stages of pupillary block by the vitreous, as follows: (1) an early stage, characterized by relative block due to decreased permeability of the hyaloid face; (2) a moderate stage, with adhesions between the vitreous and sphincter pupillae referred to as sphincteric pupillary block; and (3) the irido-hyloidal stage, with extensive adhesions between the anterior hyaloid face and the entire posterior iris surface.(6)
The diagnosis requires careful history taking and identification of precipitating factors, such as those leading to pupil constriction. These factors include bright sunlight (as in the present case) or parasympathomimetics such as pilocarpine. The presence of vitreous at the pupil axis should raise concern about the possibility of future pupil block. Pupil block glaucoma is very unusual in the presence of a patent iridectomy.
The patient was managed with medical treatment, including topical atropine until the definitive surgical treatment. A laser iridotomy might also have broken the pupil block, but the iris can be edematous with high IOP preventing a straightforward laser iridotomy.
A change in the nature of symptoms should alert the treating physician to look for pathology other than migraine to explain the nature of the symptoms.
Acknowledgments
Supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
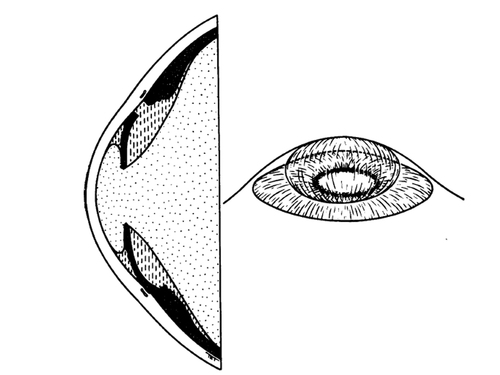
Figure 2
Cross-section and diagrammatic three-dimensional view indicating relationships between vitreous, aqueous and iris in aphakic pupil block.1 (Reproduced with permission from Hitchings RA. Acute aphakic pupil block glaucoma: an alternative surgical approach. Br J Ophthalmol 1979;63:31-7.)
Cross-section and diagrammatic three-dimensional view indicating relationships between vitreous, aqueous and iris in aphakic pupil block.1 (Reproduced with permission from Hitchings RA. Acute aphakic pupil block glaucoma: an alternative surgical approach. Br J Ophthalmol 1979;63:31-7.)
2. Shaffer RN. The role of vitreous detachment in aphakic and malignant glaucoma. Trans Am Acad Ophthalmol Otol 1954;58:217.
3. Shindler KS, Sankar PS, Volpe NJ, Piltz-Seymour JR. Intermittent headaches as the presenting sign of subacute angle closure glaucoma. Neurology 2005;65:757-8.
4. Maggioni F, Dainese F, Mainardi F, Lisotto C, Zanchin G. Intermittent angle-closure glaucoma in the presence of a white eye,posing as retinal migraine. Cephalgia 2005;25:622-6.
5. Nosher R, Hering-Hanit R, Nesher G. Subacute glaucoma masquerading as migraine: how to avoid the pitfall and make the diagnosis. Postgrad Med 2006;119:70-3.
6. Posner A. Postcataract glaucoma associated with shallow anterior chamber. Int Ophthalmol Clin. 1964;4:1029-43.