A 54-year-old woman with bluish discoloration of her sclera
Digital Journal of Ophthalmology 2010
Volume 16, Number 2
May 8, 2010
DOI: 10.5693/djo.03.2010.02.002
Volume 16, Number 2
May 8, 2010
DOI: 10.5693/djo.03.2010.02.002
Download PDF
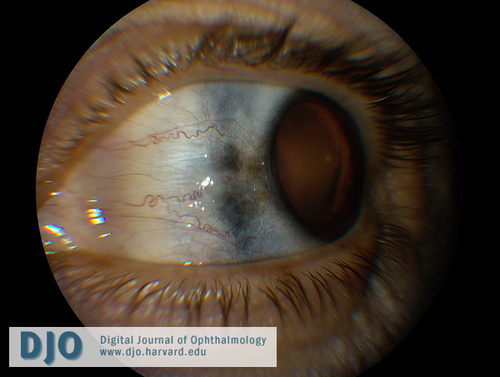
Figure 1
Left eye with bluish-gray scleral hyperpigmentation nasally.
Left eye with bluish-gray scleral hyperpigmentation nasally.
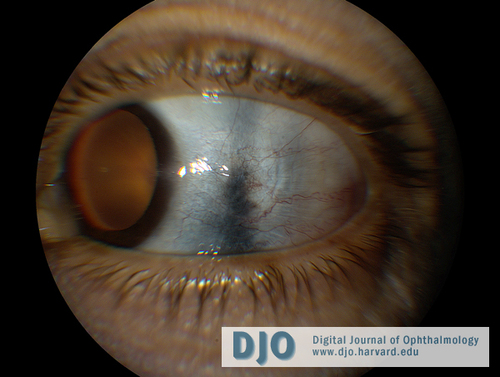
Figure 2
Left eye with bluish-gray scleral hyperpigmentation temporally.
Left eye with bluish-gray scleral hyperpigmentation temporally.
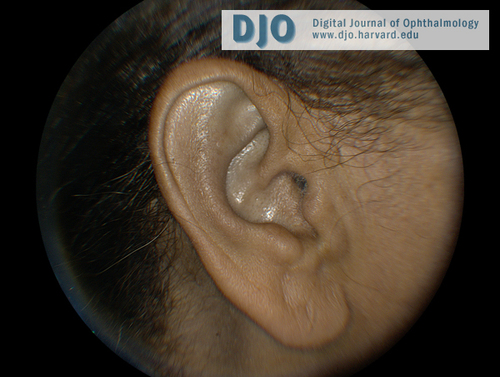
Figure 3
Bluish discoloration of the patient’s left ear.
Bluish discoloration of the patient’s left ear.
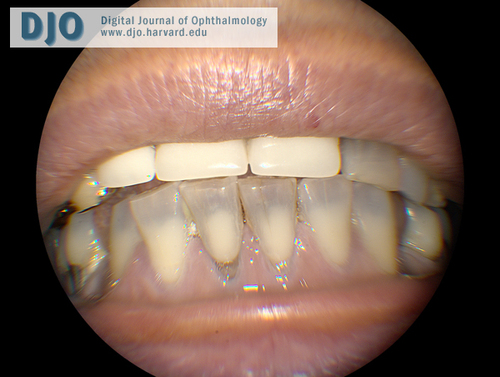
Figure 4
Bluish discoloration of the patient’s teeth and gums.
Bluish discoloration of the patient’s teeth and gums.
2. Scleromalacia is on the differential for sclera hyperpigmentation; however, this patient had no history of autoimmune disease and denied any eye or joint pain. On examination, her sclerae were not thinned and she had no conjunctival injection or uveitis. Rheumatologic work-up was negative for RF and ANA.
3. Choroidal or ciliary body melanomas can cause scleral hyperpigmentation, particularly if they invade through the sclera. Scleral invasion due to choroidal melanoma would be an indication for enucleation; however, retinal examination revealed no choroidal masses in this patient.
4. Addison’s disease can cause a bronze hyperpigmentation of the sclera. Our patient denied any weakness, fatigue, anorexia, or abdominal pain.
5. Ochronosis, or skin discoloration due to alkaptonuria, can cause a bluish-black discoloration of the ear and sclera. The patient denied any black discoloration of her urine, as would be expected in alkaptonuria so no further urine testing was performed. Serum homogentisic acid was normal.
Minocycline is a semisynthetic tetracycline used in the treatment of acne vulgaris, rosacea, and as an adjunctive medication for rheumatoid arthritis. It has also been reported to cause hyperpigmentation in the skin,(2) ears, nails,(3) teeth,(4) bones,(5) conjunctiva and sclera.(3,4,6) The scleral hyperpigmentation is often blue-gray, perilimbal, and may be more prominent in sun-exposed areas.(3,6) In the skin, hyperpigmentation is thought to be due to insoluble complexes of minocycline or minocycline derivatives with iron-related substances or calcium within macrophages of the dermis or epidermis.(7)
Cutaneous hyperpigmentation results from prolonged (greater than 2 years) use of high-dose (greater than 100 mg/day or a total of over 100 g) minocycline.(3,6) Our patient had taken a total of 1460 grams of minocycline. Skin hyperpigmentation may fade with discontinuation of the drug, particularly if the discoloration is recognized immediately,(6) but occasionally the hyperpigmentation may be permanent.(4) Cutaneous hyperpigmentation is an indication for discontinuing minocycline.(4,6) Our patient had coincidentally stopped minocycline use 2 years prior to presentation but continued to have persistent and stable scleral, ear, and gingival hyperpigmentation, suggesting that her hyperpigmentation is permanent.
Patients with minocycline-induced scleral hyperpigmentation present with a painless, blue scleral discoloration. These patients are otherwise healthy, with no other signs of systemic disease. Since this is a diagnosis of exclusion, all other causes of scleral hyperpigmentation must be considered and excluded. Scleral hyperpigmentation due to minocycline is treated with medication cessation. However, some cases of very prolonged high-dose minocycline use, as in our patient, may have permanent and irreversible pigment changes. Recognition of minocycline toxicity as a cause of scleral hyperpigmentation is key in preventing a patient from receiving systemic immunosuppression, particularly when other signs of scleromalacia are absent.
2. McGrae JD, Jr., Zelickson AS. Skin pigmentation secondary to minocycline therapy. Arch Dermatol 1980;116(11):1262-5.
3. Wolfe ID, Reichmister J. Minocycline hyperpigmentation: skin, tooth, nail, and bone involvement. Cutis: cutaneous medicine for the practitioner 1984;33(5):457-8.
4. Morrow GL, Abbott RL. Minocycline-induced scleral, dental, and dermal pigmentation. Am J Ophthalmol 1998;125(3):396-7.
5. Rumbak MJ, Pitcock JA, Palmieri GM, Robertson JT. Black bones following long-term minocycline treatment. Arch Pathol Lab Med 1991;115(9):939-41.
6. Fraunfelder FT, Randall JA. Minocycline-induced scleral pigmentation. Ophthalmology 1997;104(6):936-8.
7. Fenske NA, Millns JL. Cutaneous pigmentation due to minocycline hydrochloride. J Am Acad Dermatol 1980;3(3):308-10.