Orbit/Oculoplastics Quiz 21: A 16 Year Old Boy With Periorbital Headaches

Figure 1
Clinical appearance at presentation. There is mild edema of the right upper eyelid.
Clinical appearance at presentation. There is mild edema of the right upper eyelid.

Figure 2
CT scan at the time of presentation. There is a predominantly lytic lesion of the right frontal bone.
CT scan at the time of presentation. There is a predominantly lytic lesion of the right frontal bone.
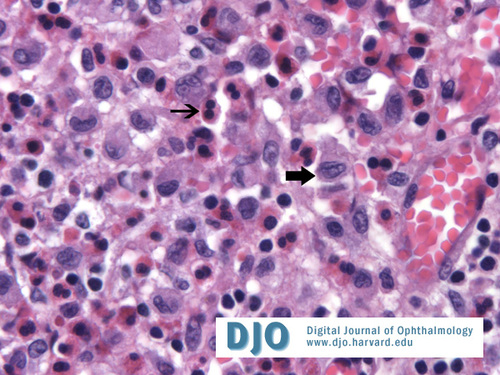
Figure 3A
There are numerous large histiocytes with folded nuclei and abundant cytoplasm (large arrow) associated with eosinophils (small arrow) infiltrating connective tissue.
There are numerous large histiocytes with folded nuclei and abundant cytoplasm (large arrow) associated with eosinophils (small arrow) infiltrating connective tissue.
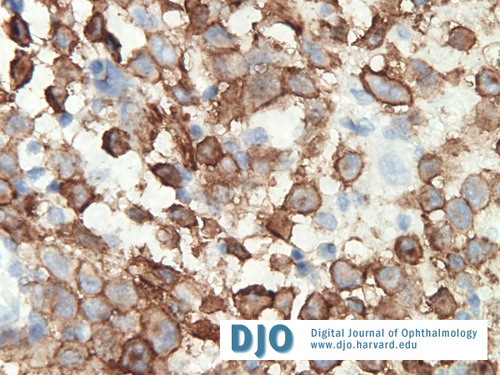
Figure 3B
The histiocytes stain positively for CD1a.
The histiocytes stain positively for CD1a.
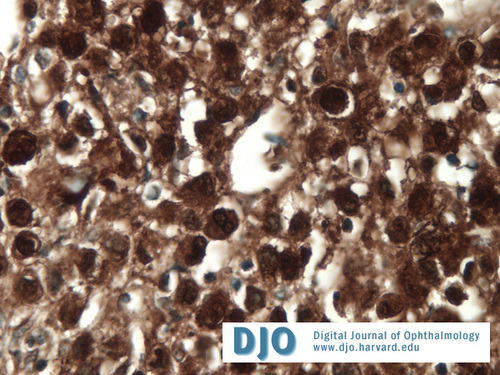
Figure 3C
The histiocytes stain positively for S100.
The histiocytes stain positively for S100.

Figure 4
CT scan of the orbits 4 months after surgical biopsy and curettage. There is new bone formation at the site of the lesion, consistent with interval healing.
CT scan of the orbits 4 months after surgical biopsy and curettage. There is new bone formation at the site of the lesion, consistent with interval healing.
Answer: The differential diagnosis includes:
-Granulomatous bone diseases such as eosinophilic granuloma (Langerhans cell
histiocytosis), cholesterol granuloma, and giant cell reparative granuloma.
-Primary bone tumors such as osteosarcoma, ossifying fibroma, and fibrous dysplasia.
-Metastatic tumors such as neuroblastoma and Ewing sarcoma.
-Other: hematic cyst, dermoid cyst.
-One must also consider lacrimal gland neoplasms if the lacrimal gland is abnormal.
2. How would you diagnose this patient?
Answer: This patient underwent a surgical biopsy and subtotal curettage. In this case, the biopsy was consistent with an eosinophilic granuloma.
Histiocytic tumors account for approximately 7% of orbital tumors in children. Langerhans cells are a type of antigen presenting cell. Langerhans cell histiocytosis (LCH) refers to a disease process in which there is a pathologic accumulation of these cells. LCH is actually a term that encompasses three related disorders: eosinophilic granuloma, Hand-Schüller-Christian disease, and Letterer-Siwe disease. Eosinophilic granuloma represents about 70% of cases of LCH. This is the most benign form of LCH and is usually characterized by solitary skeletal lesions. Hand-Schüller-Christian disease affects approximately 20% of people with LCH. It is a multifocal disease resulting in bony lesions, hepatosplenomegaly, and lymphadenopathy. The classic triad of bone destruction, exophthalmos, and diabetes insipidus is seen in about 30% of cases. Letterer-Siwe disease is the least common but most malignant form of LCH. It is an acute, disseminated disease that includes involvement of the skin, spleen, and liver. For this discussion, we will focus on orbital eosinophilic granuloma.
Patients with orbital eosinophilic granuloma tend to be males in their first or second decade. Patients present with upper eyelid edema and erythema, bone pain, and tenderness. A destructive bone lesion is commonly seen in the superior or superotemporal orbit. The pathogenesis of eosinophilic granuloma is unclear. It has been proposed that it is a reaction to a viral infection. Tissue biopsy is necessary for a diagnosis (Figure 3A). CD1a positivity (Figure 3B), S-100 positivity (Figure 3C), and the presence of Birbeck granules on electron microscopy can help to confirm the diagnosis. There are no histological differences between unifocal and multifocal disease.
While a biopsy is necessary for a diagnosis and to rule out a malignancy, there are no definitive recommendations on how best to manage a case of unifocal, orbital eosinophilic granuloma. Complete surgical removal of the lesion is not necessary. There are many reports of complete resolution of an orbital eosinophilic granuloma after biopsy and subtotal curettage alone. In these cases, it is unclear if the biopsy and curettage had a therapeutic impact or if the lesions would have spontaneously resolved without any intervention at all. Successful interventions have also been reported with the use of low-dose radiation and intralesional corticosteroids. Chemotherapy is considered when there is multifocal disease and also has been used for recurrent, unifocal disease.
3. How should a systemic workup be performed?
Answer: A systemic workup should be done to rule out multifocal disease. The patient should receive a chest xray, skeletal survey, complete blood count, liver function tests, coagulation studies, and urine specific gravity to screen for diabetes insipidus. These studies should be done in conjunction with a pediatric oncologist.
4. How should one follow the patient?
Answer: The patient should be followed for at least several years. The patient should receive serial CT scans of the orbit to watch for resolution and to monitor for recurrence. 4 months after this patient’s biopsy and curettage, the CT scan demonstrates bone remodeling and no evidence of recurrence (Figure 4).
References:
Demirci H, Shields CL, Shields JA, et al. Bilateral Sequential Orbital Involvement by Eosinophilic Granuloma. Archives of Ophthalmology 2002; 120:978-979.
Kramer TR, Noecker RJ, Miller JM, et al. Langerhans Cell Histiocytosis with Orbital Involvement. American Journal of Ophthalmology 1997; 124:814-824.
Song A, Johnson TE, Dubovy SR, et al. Treatment of Recurrent Eosinophilic Granuloma with Systemic Therapy. Ophthalmic Plastic and Reconstructive Surgery 2003; 19:140-144.
Woo KI and Harris GJ. Eosinophilic Granuloma of the Orbit: Understanding the Paradox of Aggressive Destruction Responsive to Minimal Intervention. Ophthalmic Plastic and Reconstructive Surgery 2003; 19: 429-439.