Orbit/Oculoplastics Quiz 12
Answer: Solar Lentigo
Lentigo maligna
Lentigo maligna melanoma
To the ophthalmically-based clinician, these lesions can be though to be analogous to the spectrum of acquired pigmented lesions of the conjunctiva comprising: primary acquired melanosis (PAM), PAM with atypia, and PAM with microinvasive melanoma.
2. What are the clinical and histological features of this lesion?
Answer: Lentigo (derived from the latin word lentil or lens –shaped), is a brown spot consisting of an increased number of epidermal melanocytes.
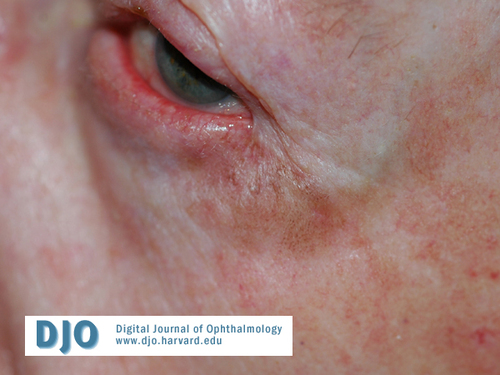
Solar lentigo (“age spots” or “liver spots”) are benign, melanotic flat lesions similar to freckles but are usually larger and persistent through the winter, and more common in older patients. Lentigo typically appears as a flat, tan-brown lesion sometimes with irregular mottling Change in pigmentation, growth in size, and, occasionally, elevation are uncommon in solar lentigo and should raise concern for lentigo maligna or lentigo maligna melanoma.
Lentigo maligna (LM) first described by Sir John Hutchinson in 1890 (and therefore also known as Hutchinson melanotic freckle) is now understood as an invasive melanoma precursor lesion of atypical melanocytic proliferation confined to the epidermis which can progress to invade the dermis, thereby becoming lentigo maligna melanoma (LMM).
Histology of LM is remarkable for an increased number of atypical melanocytes in the basal epidermis. These melanocytes typically contain spindle or stellate shaped hyperchromatic nuclei and can be multinucleated. Of note, biopsy of the darkest portion of the lesion is recommended to secure the diagnosis.
The average age of onset is in the 7th decade of life for LM and 8th decade for LMM. Both lesions typically appear on head and neck with predilection for cheek and nose and are believed to be connected to chronic solar exposure. Known risk factors include a history of severe sunburns, fair skin, and an increased number of melanocytic nevi.
3. What is the risk of malignant transformation?
Answer: The risk of transition from LM to LMM by invasion of the dermis is unknown. This process appears to occur over long periods of time (5 to 15 years) and some publications estimate the lifetime risk of progression from 2 to 5 %.
4. What tools can help to identify the margins of the lesion?
Answer: Traditionally a Wood’s light (UVA, “black lamp”) has been used estimate the extent of the lesion by providing a heightened contrast between the pigmented areas in which the UV light is preferentially absorbed by epidermal melanin and surrounding uninvolved tissue. More recently, Digital Epiluminesence Microscopy, providing 30-fold magnification, has been used to ease the delineation of pathologic borders.
5. What are the treatment options?
Answer: The definitive treatment of lentigo maligna is surgical excision. The recommended margins of 5 mm can be inadequate due to the subclinical extension of the lesion into surrounding tissue.
Although Mohs’ micrographic surgery (MMS) is useful for non-pigmented lesions, determination of the extent of pigmented lesions based solely on frozen sections may not be accurate. Instead, the “slow Mohs” technique has become the preferred technique in which the surgical margin are inspected after rush permanent fixation with staged excision on consecutive days followed by repair of the resulting wound.
Cryo-, laser-, and radio-therapy have been described but are not recommended due to the inability to ensure complete removal of the lesion. Medical treatment by intralesional interferon alpha injections has shown regression of LM in some cases and recently topical immunomodulation with imiquinod cream (Aldara) has shown promising results but must be considered experimental at this time.
6. References:
Arlette JP, Trotter MJ, Trotter T, Temple CL. Management of lentigo maligna and lentigo maligna melanoma: seminars in surgical oncology. J Surg Oncol. 2004 Jul 1;86(4):179-86.
Barlow RJ, White CR, Swanson NA. Mohs' micrographic surgery using frozen sections alone may be unsuitable for detecting single atypical melanocytes at the margins of melanoma in situ. Br J Dermatol. 2002 Feb;146(2):290-4.
Robinson JK. Use of digital epiluminescence microscopy to help define the edge of lentigo maligna. Arch Dermatol. 2004 Sep;140(9):1095-100.