Glaucoma Quiz 3
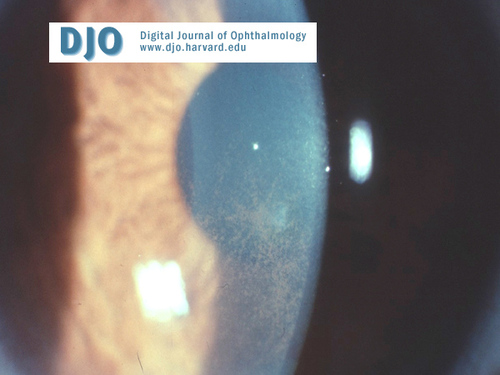
Figure 1
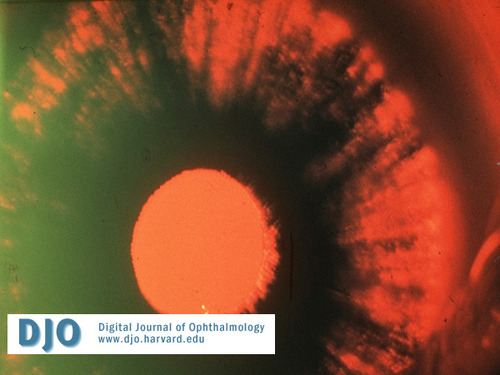
Figure 2
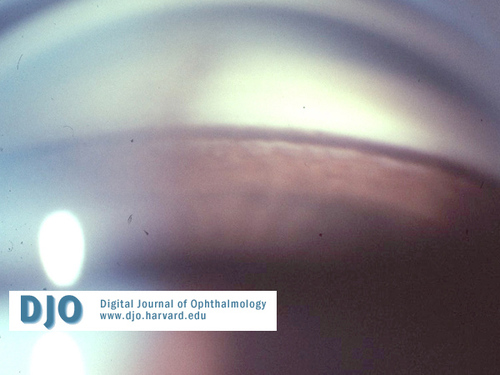
Figure 3
Answer: Figure 1 shows deposition of pigment on the corneal endothelium in a vertically oval spindle-pattern called Krukenberg's spindle. This specific pigment pattern results from aqueous convection currents.
2. What is the condition called if there is no associated glaucoma?
Answer: Pigment dispersion syndrome. These patients are at 25%-50% risk of developing pigmentary glaucoma and need life-long surveillance for glaucoma.
3. What are the diagnostic signs of this glaucoma?
Answer: Besides the increased intraocular pressure (IOP), optic nerve cupping and visual field changes, the classic triad of pigmentary glaucoma consists of Krukenberg's spindle (Figure 1), mid-peripheral radial iris transillumination defects (Figure 2), and dense pigment deposition over the trabecular meshwork (Figure 3). A Scheie's stripe, or pigment deposition on the peripheral posterior lens capsule, may also be seen. Any patient coming in for a routine eye exam should be checked for iris transillumination defects.
4. What is the pathogenesis of glaucoma in these patients?
Answer: Abnormal posterior bowing of the iris allows the posterior iris pigment epithelium to rub against the lens zonules. Pigment is thus released and deposited throughout the anterior segment (i.e. the corneal endothelium, trabecular meshwork, iris surface, zonules, peripheral lens capsule, anterior vitreous face, etc.). Pigmentary glaucoma may partly be caused by this pigment deposition in the trabecular meshwork, whose increased resistance to the aqueous outflow results in IOP elevation.
5. What are the predisposing factors?
Answer: Pigment dispersion/pigmentary glaucoma can be seen in young, myopic, Caucasian males. Exercise may increase pigment release. Pigment dispersion may be associated with a reverse pupillary block mechanism. There may be multiple genetic factors.
6. What is the differential diagnosis?
Answer: This condition should be differentiated from pseudoexfoliative glaucoma and the uveitic glaucomas, as well as from transillumination defects from either senile changes or malpositioned posterior chamber intraocular lenses.
7. What is the treatment for these patients?
Answer: For pigmentary glaucoma patients, glaucoma medications may be used as in primary open-angle glaucoma. Argon laser trabeculoplasty (ALT) may be effective in lowering IOP. Caution should be exercised when choosing the energy level for ALT. It is controversial whether peripheral laser iridotomy should be used to minimize the posterior bowing of the iris in order to decrease pigment dispersion. It is also controversial whether miotics should be used since they not only constrict the pupil and minimize irido-zonular contact and thereby decrease pigment release but also preclude a good view of the peripheral retina in a probable myope. Patients with pigment dispersion syndrome must be seen regularly to screen for glaucoma.
