Glaucoma Quiz 5
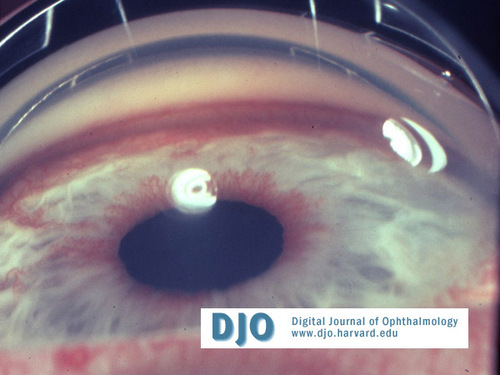
Figure
Answer: Neovascular glaucoma (NVG).
2. What is the pathogenesis of this condition?
Answer: Severe retinal ischemia stimulates the production of angiogenic factors that result in neovascularization of the iris (NVI) and the angle. As the new blood vessels arborize over the surface of the iris and the angle, a fibrovascular membrane is formed. The fibrovascular membrane obstructs the aqueous outflow causing secondary open-angle glaucoma. This is followed by the contraction of the fibrovascular membrane in the angle, which causes peripheral anterior synechiae and secondary angle-closure glaucoma. Radial traction along the surface of the iris pulls the pigment layer around the pupillary margin anteriorly, causing ectropion uveae.
3. What are the different stages?
Answer: Stage 1: Neovascularization on the iris surface, the pupillary margin, and/or the trabecular meshwork. The angle is open and the IOP is normal.
Stage 2: Stage 1 with increased intraocular pressure. A fibrovascular membrane is formed over the angle. By gonioscopy, the angle appears open and the IOP is raised (secondary open-angle glaucoma).
Stage 3: The fibrovascular membrane contracts and forms peripheral anterior synechiae. Secondary angle-closure glaucoma results.
4. What are the etiologic factors?
Answer: Diabetic retinopathy (one third) and central retinal vein occlusion (CRVO) (one third) are the two most common causes of anterior segment neovascularization. Other causes are carotid artery occlusive disease (10-15%), central retinal artery occlusion (CRAO), branch retinal vein occlusion (BRVO), uveitis, chronic retinal detachment, intraocular tumors, trauma, and radiation.
5. What is the work-up of patients with this disease?
Answer: The cause of neovascularization must be found. A complete medical and eye examination must be done. A B-scan ultrasound is done if the retina cannot be visualized to rule out any intraocular pathology. Fluorescein angiography may further define any retinal abnormalities. Carotid studies and cardiac evaluation are done if no retinal abnormalities are found.
6. What is the differential diagnosis?
Answer: Dilatation of iris vessels after surgery or uveitis, pseudoexfoliative glaucoma, essential iris atrophy, Fuch’s heterochromic iridocyclitis, acute angle-closure glaucoma, congenital iris tufts, retinopathy of prematurity, carotid cavernous fistula, and prominent iris vessels in lightly pigmented eyes.
7. How do you treat this case?
Answer: Medical treatment may include beta-blockers, alpha adrenergic agonists, carbonic anhydrase inhibitors, atropine, and corticosteroids. Treatment of the underlying disease may include panretinal photocoagulation (PRP), as in proliferative diabetic retinopathy or central retinal vein occlusion. Cryoablation (or cryotherapy) may be done if the retina cannot be visualized. If medical treatment and PRP fails, filtration surgery with antimetabolites, tube shunt surgery, or cyclodestruction may be done.