Glaucoma Quiz 8
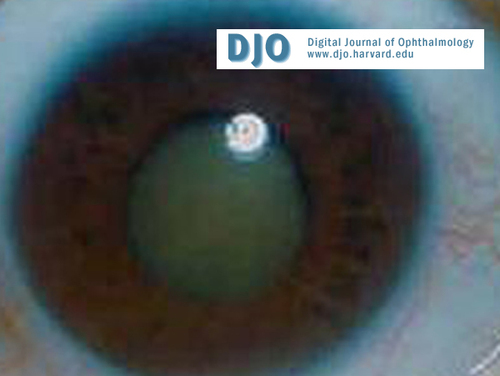
Figure 1
Phacomorphic Glaucoma
Phacomorphic Glaucoma
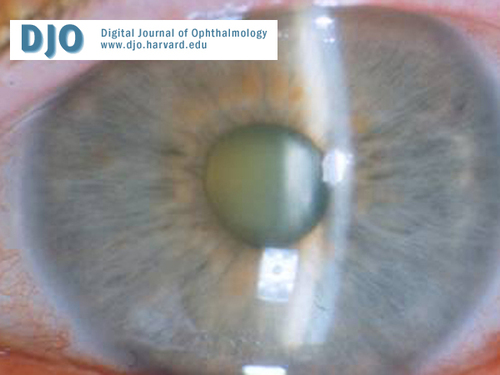
Figure 2a.
Phacomorphic glaucoma.
Phacomorphic glaucoma.
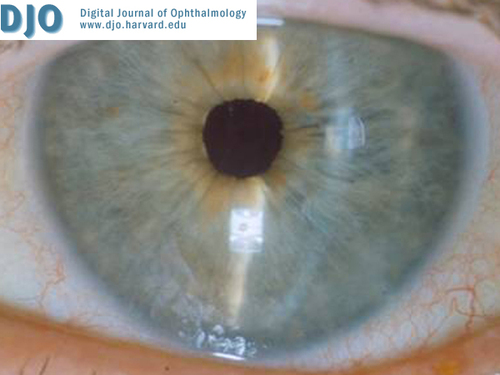
Figure 2b.
Same eye after cataract surgery.
Same eye after cataract surgery.

Figure 3.
Phacolytic glaucoma.
Phacolytic glaucoma.

Figure 4.
Lens particle glaucoma.
Lens particle glaucoma.

Figure 5.
Lens displacement.
Lens displacement.
Answer: Phacomorphic Glaucoma.
2. How do you differentiate this condition from acute primary angle-closure glaucoma?
Answer: Phacomorphic glaucoma initially causes pupillary block as a result of a swollen, intumescent lens. Therefore, the anterior chamber is very shallow. In later stages, there is direct appositional closure of the angle from the lens pushing the peripheral iris anteriorly. Phacomorphic glaucoma is usually unilateral. The other eye may have a normal anterior chamber depth. The other eye may also not be classically hyperopic, as with primary angle closure glaucoma. The definitive cure for phacomorphic glaucoma is cataract surgery. The definitive cure for acute primary angle closure glaucoma is peripheral iridotomy.
3. What is the treatment of this condition?
Answer: Medical treatment is used to decrease the inflammation and to lower the IOP. Laser peripheral iridotomy may also be considered to help lower the pressure in order to allow more time for topical steroids to minimize inflammation prior to cataract surgery. The definitive treatment is cataract surgery (Figure 2a and 2b). Trabeculectomy surgery is usually not needed.
4. What is phacolytic glaucoma?
Answer: With a mature or hypermature cataract, leakage of high molecular weight lens protein through an intact capsule leads to trabecular meshwork obstruction (Figure 3). Symptoms are pain, redness, and decreased vision. Signs include increased IOP associated with corneal edema, cells/flare, occasional iridescent particles in the aqueous, macrophage aggregates on the anterior lens capsule, and an occasional pseudo-hypopyon. In contrast to phacomorphic glaucoma, the angle is gonioscopically open and the anterior chamber may be deep.
5. What is lens particle glaucoma?
Answer: This may occur after acute penetrating injury or after cataract surgery with retained lens material ( Figure 4). The lens or cortical material and the inflammatory cells may then block outflow. If medical treatment (i.e. glaucoma medications, cycloplegics, and steroids) does not control the intraocular pressure, surgical removal of the lens material is needed.
6. What is phacoantigenic glaucoma?
Answer:
This usually presents as an intractable uveitis due to lens protein liberated by lens capsule disruption. Patients become sensitized to their own lens protein, and the resulting uveitis may initially cause low IOP. Less commonly, inflammatory deposits may occlude the trabecular meshwork and increase the IOP. Later stages may be associated with peripheral anterior synechiae and glaucoma. Trauma or extracapsular cataract extraction (ECCE) may be the triggering events. Pathology shows zonal granulomatous inflammation. Treatment may include reduction of the inflammation and IOP. Definitive treatment is removal of all residual lens material.
7. What is lens-displacement glaucoma?
Answer: A displaced lens may mechanically obstruct the passage of aqueous through the pupil causing pupillary block and secondary angle-closure glaucoma. Lens displacement may occur because of trauma, congenital anomalies [e.g. Marfan’s syndrome (Figure 5)], homocystinuria, Weill-Marchesani syndrome, and others.