A 65-year-old man with decreased vision OD
Digital Journal of Ophthalmology 2008
Volume 14, Number 11
June 15, 2008
Volume 14, Number 11
June 15, 2008
He had a history of hypertension, hyperlipidemia (both controlled with medication), myocardial infarction and intermittent claudication (for which he had undergone bilateral ileofemoral bypass and was currently on warfarin). He smoked 20 cigarettes per day.
There was no significant past ocular history.
He had a family history of hypertension, hyperlipidemia and myocardial infarction.
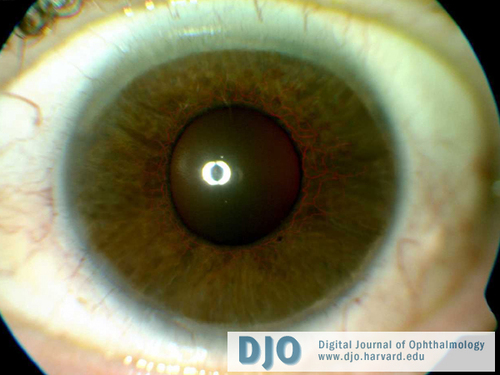
Figure 1
Anterior segment photograph of the right eye demonstrating iris neovascularization
Anterior segment photograph of the right eye demonstrating iris neovascularization

Figure 2
Posterior segment photograph of the right eye displaying midperipheral dot and blot hemorrhages and scars from pan retinal photocoagulation
Posterior segment photograph of the right eye displaying midperipheral dot and blot hemorrhages and scars from pan retinal photocoagulation
Despite the above treatment and maximum topical anti glaucoma medication over the next 8 months, the NVI failed to regress and the IOP gradually increased to 50 mm Hg. The eye, however, remained comfortable. The left eye was unaffected.
The patient was lost to follow-up for 4 months. He then presented to the casualty service with complaints of recurrent episodes of sudden, painless loss of vision in the left eye for one week. He reported that the vision usually returned to normal within a few minutes to half an hour. There was no associated headache, neck pain, myalgia, jaw claudication (suggestive of giant call arteritis) or nausea and vomiting.
On examination, his blood pressure was within normal limits. Visual acuities were no light perception (NLP) OD and 20/40 OS. He had bilateral cataracts (mature in OD), severe NVI and high IOP (50 mm Hg OU). The left eye showed advanced optic disc cupping with visible spontaneous retinal arterial pulsation. The right fundus was not visualised due to a dense cataract.
His treatment was similar to that given for the right eye; specifically, he received intravenous, oral and topical anti-glaucoma agents, topical steroids, argon-laser iridoplasty, Nd:Yag laser iridotomies and extensive PRP.
Carotid angiography revealed 100% stenosis of right internal carotid artery and 80% stenosis of left internal carotid at its origin (Figure 4). He was advised to stop smoking and was offered carotid endarterectomy with 50% risk of major complications such as stroke or death. The patient elected to proceed and had successful surgery with a saphenous vein patch.
Post-operatively, his IOP OS remained at 50 mm Hg along with intermittent visual obscurations and visible central retinal arterial pulsations. Accordingly, trabeculectomy was performed with Mitomycin C (0.2mg/ml) and two releasable sutures. A surgical peripheral iridectomy was not fashioned due to the risk of hemorrhage from the florid NVI; intentionally a large Nd:YAG peripheral iridotomy was positioned immediately beneath the bleb.
On follow up examination, both eyes were comfortable. Visual acuity OS was 20/63 with an IOP of 10 mm Hg without anti glaucoma medication. Visual acuity OD remained NLP with an IOP of 55 mm Hg despite ongoing treatment with topical prostaglandin analogues (Latanoprost 0.005%), alpha-2 agonist (Brinzolamide 1%) and beta blocker (Timolol 0.5%).
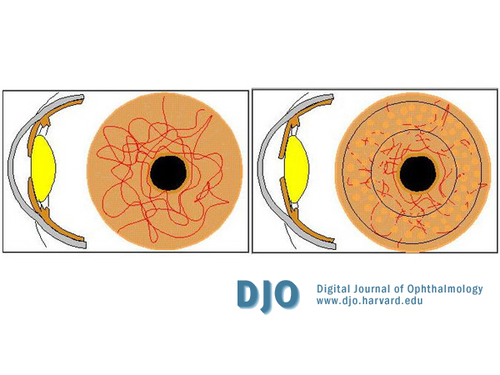
Figure 3
360-degree Argon laser iridoplasty to tighten the iris, open up the angles of the anterior chamber and ablate the NVI
360-degree Argon laser iridoplasty to tighten the iris, open up the angles of the anterior chamber and ablate the NVI
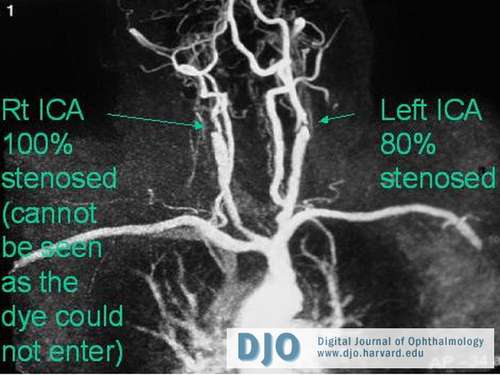
Figure 4
Carotid angiography showed 100% stenosis of right internal carotid artery and 80% stenosis of left internal carotid at its origin
Carotid angiography showed 100% stenosis of right internal carotid artery and 80% stenosis of left internal carotid at its origin
Diabetic retinopathy is usually bilateral, symmetric and tends to be confined to the posterior pole as opposed to the mid periphery. In addition, hard exudates are also found which are absent in OIS.
Aortic arch disease caused by atherosclerosis, syphilis or Takayasu arteritis produces a clinical picture identical to OIS, and is usually bilateral. Examination reveals absent arm and neck pulses, cold hands, and spasm of the arm muscles with exercise.
OIS can rarely occur secondary to inflammatory vasculitis caused by giant cell arteritis of the ophthalmic artery. As such, in patients over the age of 55, a review of systems addressing jaw claudication, scalp tenderness, and constitutional symptoms should be explored. If there is adequate clinical suspicion, further workup for GCA should be pursued.
Symptoms of OIS include visual loss, amaurosis fugax, prolonged recovery of vision after exposure to bright light and ocular or periorbital pain.(3) It typically occurs in patients aged 50-80 years; men are more frequently affected than women.
Ocular examination reveals NVI, elevated IOP, uveitis, retinal arteriolar narrowing, dilated retinal venules, characteristic mid-peripheral retinal dot and blot hemorrhages and posterior segment neovascularisation. Fluorescein angiogram can show delayed and patchy choroidal filling, prolongation of the arteriovenous transit time, staining of the retinal vessels, macular edema, retinal capillary nonperfusion, and neovascularization of the disc or elsewhere.(1,2,4,5) OIS may also be associated with neurological symptoms such as stroke, or it may be the sole manifestation of carotid occlusive disease.
Management of patients with suspected OIS involves:
1. Examination of the cardiovascular system and evaluation for hypertension, diabetes and atherosclerotic disease.
2. The carotid artery system can be studied with noninvasive carotid ultrasound, which has an accuracy of around 95% in detecting carotid artery stenosis of 75% or more at the bifurcation.(6) Transcranial Doppler images the ophthalmic artery and documents any reversal of blood flow. Magnetic resonance imaging, magnetic resonance angiography and carotid angiography show the entire extent of the carotid system and its branches and additionally helps to identify intracranial lesions.
3. Treatment of OIS remains difficult and controversial. Since internal carotid artery occlusive disease is the most common cause, carotid endarterectomy (CEA) would seem a logical management; however, the benefit to patients is unknown and controversial.(7) CEA is usually offered if the stenosis is >70%. Intracranial carotid artery disease with stenotic lesions above the second cervical vertebrae (C2) are not amenable to surgical intervention. Carotid artery angioplasty with stenting has shown to improve cerebral perfusion(8) in these cases, resulting in improvement in ophthalmic artery blood flow and FA filling times.
Standard therapy includes treatment of the underlying ischemic stimulus, typically with PRP combined with medical and surgical management of the elevated intraocular pressure. Topical steroids are used to decrease associated inflammation; cycloplegics may be useful to decrease ciliary pain and prevent posterior synechiae. Since perfusion pressure (mean blood pressure minus IOP) in the various ocular vascular beds is diminished, lowering IOP as much as possible is crucial to improve the blood flow and reduce the risk of retinal and optic nerve head ischemic visual loss. In addition, it is important to avoid any drop in systemic blood pressure, particularly nocturnal arterial hypotension, to prevent visual loss.(9,10) For this reason, the use of topical â-blocker eye drops to lower IOP is contraindicated in these eyes because they may produce significant nocturnal arterial hypotension, which can be visually deleterious.(11)
VEGF levels have been shown to be elevated in the vitreous in many pathological conditions that lead to neovascular glaucoma, as well as in the aqueous of patients with active neovascular glaucoma.(12) Anti-VEGF drugs offer the possibility of rapid regression of anterior segment neovascularization in an effort to avoid complete angle closure. There have been several reports of rapid regression of rubeosis following intravitreal bevacizumab in neovascular glaucoma.(13,14,15) However, this is not without potential local and systemic side effects. To date, there is no comprehensive study providing definitive information for long-term control of ocular neovascularization and neovascular glaucoma, and the complications of anti-VEGF therapy. In practice, PRP is still used as standard first line therapy and can be supplemented with intravitreal bevacizumab as a temporizing measure to prevent complete angle closure while awaiting the effect of PRP.
OIS has a poor visual prognosis and is often difficult and frustrating to treat. The ophthalmologist’s diagnosis may be crucial to the health of these patients as OIS may be the presenting sign of serious cerebrovascular and ischemic heart disease. Further studies are required to document role of CEA and anti-VEGF therapy in OIS.
2. Young L H, Appen R E. Ischemic oculopathy: A manifestation of carotid artery disease. Arch Neurol. 1981;38:358–366.
3. Kunimoto DY, Kanitkar K D, Makar M S. The Wills Eye Manual Fourth Ed. Ocular Ischaemic Syndrome. Philadelphia: Lippincott Williams &Wilkins, 2004; chap 11.10.
4. Mizener J B, Podhajsky P, Hayreh S S. Ocular ischemic syndrome. Ophthalmology. 1997;104:859–864.
5. Sarkies N J, Shilling J S and Russell R W. Fluorescein angiography in carotid disease. Trans Ophthalmol Soc U K. 1986;105:489–493.
6. Castaldo J E, Nicholas G G, Gee W, Reed JF. Duplex ultrasound and ocular pneumoplethysmography concordance in detecting severe carotid stenosis. Arch Neurol. 1989;46:518–522.
7. Mizener JB, Podhajsky P, Hayreh SS. Ocular ischemic syndrome. Ophthalmology. 1997;104:859–864.
8. Wholey M H, Wholey M. Current status in cervical carotid artery stent placement. J Cardiovasc Surg (Torino). 2003;44:331–339.
9. Hayreh SS, Zimmerman MB, Podhajsky P, Alward WLM. Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol. 1994;117:603–624.
10. Hayreh SS, Podhajsky PA, Zimmerman B. Role of nocturnal arterial hypotension in optic nerve head ischemic disorders. Ophthalmologica. 1999;213:76–96.
11. Hayreh SS, Podhajsky PA, Zimmerman B. â-Blocker eye drops and nocturnal arterial hypotension. Am J Ophthalmol. 1999;128:301–309.
12. Tripathi RC, Li J, Tripathi BJ, et al. Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma. Ophthalmology. 1998;105:232–237.
13. Davidorf FH, Mouser JG, Derick RJ. Rapid improvement of rubeosis iridis from a single bevacizumab (Avastin) injection. Retina. 2006;26:354–356.
14. Kahook MY, Schuman JS, Noecker RJ. Intravitreal bevacizumab in a patient with neovascular glaucoma. Ophthalmic Surg Lasers Imaging. 2006;37:144–146.
15. Mason JO 3rd, Albert MA Jr, Mays A, Vail R. Regression of neovascular iris vessels by intravitreal injection of bevacizumab. Retina. 2006;26:839–841.