A seven month old baby with a right sticky eye
Digital Journal of Ophthalmology 2006
Volume 12, Number 3
May 10, 2006
Volume 12, Number 3
May 10, 2006
A 7-month-old child attended eye casualty with a 7 week history of a right sticky eye. The mother had recently noticed excessive crusting around the lid margin, encroaching on the cornea. There was no significant medical or family history. He was otherwise fit and well. The prenatal course for the mother and child was unremarkable. The child did not take any regular medications and had no known allergies.
On examination, the child objected strongly to occlusion in their left eye. A green discharge was noted in association with a ‘fleshy’ mass extending from the upper palpebral conjunctiva to involve the visual axis of the right eye (see figure 1). A smaller lower lid membrane was also noted. The remaining ocular examination was unremarkable.
Figure 1 (fleshy mass involving upper palperbral conjunctiva of the right eye)

Figure 1 (fleshy mass involving upper palperbral conjunctiva of the right eye)
Ancillary testing
Bacterial and Chlamydial swabs: No abnormality detected
A plasminogen assay was requested. The result showed a reduced level of 0.19u/ml of plasminogen (normal: 0.80-1.20).
Pathology
The membranous sample was sent for histological and microbiological examination (figure 2): results confirmed ligneous conjunctivitis as the diagnosis
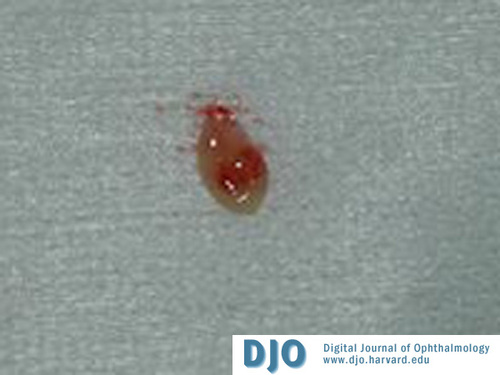
Figure 2 (the membranous sample which was sent for histological and microbiological examination)
Initially treatment with topical ofloxacin, four times a day, was commenced and attempts made to remove the membranes under topical anaesthesia. At attempted removal with forceps, the membranes began bleeding, inhibiting the view leading to the procedure to be abandoned. G Pred forte (four times a day) was added.
The child was reviewed on a weekly basis with recurrent successful attempts at debridement of the membranes. Following 4 attempts at removal of the upper lid membranes, the decision was made to anesthetise the child for complete excision. The membranes were removed and the child treated with hourly topical Heparin (1000U/ml) and hourly G. Pred forte using the regime described by De Cock et al (1).
On review 2 weeks later, the child was well. The eye was quiet, there was no longer any discharge present or any sign of membrane recurrence (figure 3). At this stage the drops were reduced slowly to 2-hourly for one week, followed by 6 times a day for one week and then four times a day for a further month. The child recovered fully after this course and was discharged.

Figure 3 showing bleeding of the lesion after removal under anaesthetic
Ligneous conjunctivitis is a rare form of idiopathic membranous conjunctivitis first reported in 1847 (2). Over 100 cases have been reported worldwide, but the true incidence remains unknown.
Although the exact etiology is unknown, local injuries, infections, lime burns and surgical interventions have all been associated with ligneous conjunctivitis (3). Most cases are sporadic although an autosomal recessive inheritance pattern has been described (4). It has since been found that ligneous conjunctivitis is strongly associated with homozygous or compound-heterozygous type I plasminogen deficiency (5).
Most often the upper tarsal conjunctiva is involved, presenting with thick viscous, mucopurlent discharge. The membranes are firm, sessile and affect both eyes in 50% of cases. Visually impairing corneal involvement may be seen in up to 30% of cases (6). The disease duration can be variable and may extend from a few months to as long as 36 years (7).
Importantly, additional sites such as the kidneys, respiratory tract, female genitalia, ear and gingival maybe involved (3).
The precise mechanism of membrane formation in ligneous conjunctivitis has been suggested to centre on the plasminogen activator system and wound healing. The mechanism behind wound healing is highly regulated to remove injured tissue and replace it with normal healing tissue. A tissue injury results in plasma protein exudation and immediate coagulation. This clot provides haemostasis and is eventually replaced by granulation tissue, which in turn is replaced by a secondary collagenous matrix. Granulation tissue degradation is dependent on the plasminogen-activator system and matrix metalloprotease (MMPs). In fact, it has been shown that patients suffering ligneous conjunctivitis, healing in mucus membranes is markedly impaired with membranes largely consisting of fibrinogen. This may signify a deficiency of extracellular fibrinolysis (3). The role of plasminogen deficiency in the pathogenesis of ligneous conjunctivitis is further supported by a case of membrane formation in a patient taking tranexamic acid, a commonly used antifibrinolytic drug (8).
Spontaneous resolution of this condition is rare (9) and several treatment modalities have been tried. In light of hypoplasminogeneaemia being a strong aetiological factor, the number of ocular surgical procedures should be kept to a minimum to prevent membrane formation in such patients. Many forms of local treatment have been used, often with disappointing results. Topical hyaluronidase has been used successfully in some patients but not all. Cyclosporine A in combination with a topical corticosteroid may decrease severity and recurrences following surgical excision, without systemic side effects (10). De Cock et al (1) showed aggressive initial treatment of membranes with surgical excision and immediate intensive topical heparin and prednisolone until complete reepithelisation of the conjunctiva controlled disease in 13/17 cases. This is the regimen we used in the presented case. Watts et al (11) showed the use of topical plasminogen concentrate in softening membranes for ease of removal.
The treatment regimen utilized in this case resulted in successful resolution of symptoms. Plasminogen deficiency was noted in the child and has been strongly associated with ligneous conjunctivitis in the literature (5, 11, 12). Hypoplasminogeneaemia may point towards a diagnosis of ligneous conjunctivitis before a formal histology report is available and is therefore an important investigation to consider in cases of membranous conjunctivitis.
1. De Cock R, Ficker LA, Dart JG, et al. Topical heparin in treatment of ligneous conjunctivitis. Ophthalmology 1995;102:1654-9
2. Bouisson M. Ophthalmie sur-aigue formation de pseudomembranes a la surface de la conjonctive. Ann Oculist 1847:17;100-4
3. Schuster V, Seregard S. Ligneous conjunctivitis. Surv of Ophthamol 2003;48:369-388
4. Francois J. Considerations on the importance of genetics in ophthalmology. Ophthalmologica 1979;178:381-95
5. Schuster V, Seidenspinner S, Zeitler P, et al. Compound heterozygous mutations in the plasminogen gene predispose to the development of ligneous conjunctivitis. Blood 1999;85:3457-66
6. Pfannkuch F, Schmidt R, Schmidt B, Seiler T. Morphological studies on the pathogenesis of ligneous conjunctivitis. Klin Monatsbl Augenkeilkd 1987;190:40-5
7. Verhoeff FH. A case of ligneous conjunctivitis now 36 years in duration. Am J Ophthalmol 1958;45:246-51
8. Diamond JP, Chandna A, Williams C, et al. Tranexamic acid –associated ligneous comjunctivitis with gingival and peritoneal lesions. Br J Ophthalmol 1991;75:753-4
9. Hidayat AA, Riddle PJ. Ligneous conjunctivitis. A clinicopathologic study of 17 cases. Ophthalmology 1987; 94:949-59
10. Holland EJ, Chan CC, Kuwabara T, et al. Immunohistologic findings and results of treatment with cyclosporine in ligneous conjunctivitis. Am J Ophthalmol 1989;107:160-6
11. Watts P, Suresh P, Mezer E, et al. Effective treatment of ligneous conjunctivitis with topical plasminogen. Am J Ophthalmol 2002;133:451-5
12. Heidemann DG, Williams GA, Hartzer M, Ohanian A, Citron ME. Treatment of ligneous conjunctivitis with topical plasmin and topical plasminogen. Cornea. 2003 Nov;22(8):760-2