|
|
44 year-old man with double vision
Digital Journal of Ophthalmology 2006
Volume 12, Number 4
December 3, 2006
|
Printer Friendly
|
|
|



Joseph Rizzo, M.D. | Harvard Medical School/Massachusetts Eye and Ear Infirmary Corey Westerfeld, M.D. | Harvard Medical School/Massachusetts Eye and Ear Infirmary
|
|
|
| History |
A 44 year-old man presents with double vision. The diplopia began 2 months ago and has not changed since that time. It is binocular, vertical, and the same at both distance and near. He denies pain. His past medical history is only significant for gastroesophageal reflux disease for which he is taking Omeprazole. His past surgical history is notable for an appendectomy at age 20. Family history and social history are noncontributory.
|
|
| Examination |
| Visual acuities are 20/20 each eye. Color plate testing is full in both eyes. Lids, anterior segment, pupillary exam, and intraocular pressures are all unremarkable. Dilated fundus examination reveals cup:disc ratios of 0.3 OU along with normal maculae, vessels, and periphery. Goldmann visual field testing was performed and was full in both eyes. Motility reveals full ductions and versions in both eyes. However, there was a left hypertropia of 4 prism diopters in primary gaze. The left hypertropia increased on right gaze to 14 prism diopters. It also increased on left head tilt to 20 prism diopters. Vertical fusional amplitude testing revealed fusional amplitudes of 8-10 prism diopters. |
|
| Ancillary Testing |
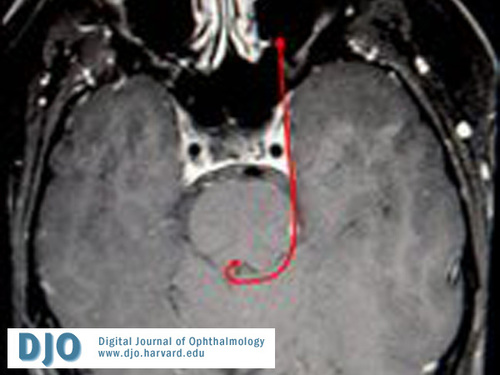
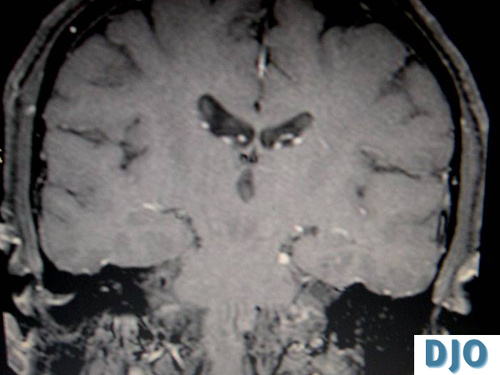
Radiographic Studies
MRI performed without contrast was normal. However, MRI with gadolinium revealed the presence of a contrast-enhancing lesion along the course of the left fourth nerve. This finding is consistent with a left fourth nerve schwannoma. |
|
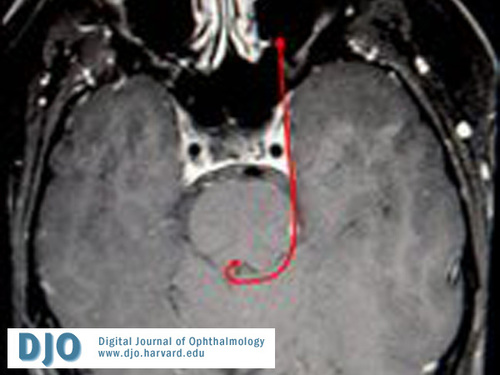
Fourth nerve schwannoma
|
|
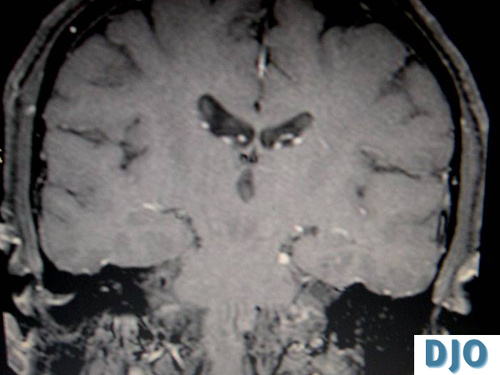
Fourth nerve schwannoma
|
|
| Treatment |
| The patient was given a prescription for a prismatic correction in his glasses. He was given 4 prism diopters base down in front of the left eye. This was placed in a trial frame in the office and was found to alleviate the diplopia in primary gaze. The option of strabismus surgery in the future was also discussed. The plan is for him to use the prisms for several months and evaluate whether or not his symptoms are sufficiently alleviated. If he remains bothered by the diplopia, in spite of the prisms, and his degree of diplopia remains stable, then surgical correction will be considered. |
|
| Differential Diagnosis |
| Fourth cranial nerve palsies must first be distinguished from other causes of vertical diplopia. These include oculomotor palsy, skew deviation, myasthenia gravis, and Graves' ophthalmopathy. These patients typically have other clinical findings that help differentiate them from isolated fourth nerve palsies. Furthermore, in time, these patients often develop other findings that unmask the diagnosis.(1) The differential diagnosis of a fourth nerve palsy can be subdivided into congenital versus acquired. Congenital fourth nerve palsies are identified in several ways. First, the patient will often have very high vertical fusional amplitudes. Normal vertical fusional amplitudes are in the range of 1-3 prism diopters. Patients with a congenital fourth nerve palsy can often fuse 10-15 prism diopters. Also, old pictures can be examined to determine whether or not there has been a long-standing head tilt since childhood. This would give more evidence to suggest that the fourth nerve palsy was congenital. When a cause can be identified, the most common etiology of an acquired fourth nerve palsy is trauma. Another common etiology is microvascular or ischemic, often in the setting of diabetes or hypertension.(2) Other etiologies include compressive lesions such as tumors or aneurysms, increased intracranial pressure, intrinsic neoplasms of the fourth nerve, and, very rarely, giant cell arteritis. |
|
| Diagnosis and Discussion |
Left fourth nerve palsy secondary to a left fourth nerve schwannoma.
Schwannomas comprise 8% of intracranial neoplasms and usually involve the 7th or 8th cranial nerves. Schwannomas may also involve the fifth cranial nerve, presenting as orbital masses in adults. They often occur in the setting of Neurofibromatosis Type II. A recent paper evaluating fourth nerve palsies reviewed 221 cases of fourth nerve palsies. 68 of the cases were found to have an isolated 4th nerve palsy. Of those, 6 were due to a radiologically identifiable 4th nerve schwannoma. A mean follow-up of 15 months found that none of the patients developed any additional symptoms or signs of cranial nerve or brainstem involvement.(3) These findings suggest that these patients can simply be followed over time with low risk of further neurologic consequence.
Interestingly, the neurosurgical literature reports many patients with fourth nerve schwannomas in association with other neurologic findings, often necessitating surgical excision.(4) It is likely that the patients who present to neurosurgeons represent a different subset of patients whose tumors are often larger and in closer proximity to brainstem structures, thus producing other signs. To date, patients who present with isolated fourth nerve palsies secondary to a schwannoma have not been shown to progress to further brainstem involvement.
Also, of note, our patient did have high vertical fusional amplitudes. We postulate that this is due to the relatively long period during which the schwannoma had been present resulting in a clinical picture similar to that of a congenital fourth nerve palsy. As such, it is possible that some portion of patients diagnosed with a “congenital” fourth nerve palsy, if imaged, would demonstrate a fourth nerve schwannoma. This does not significantly alter management, although, it does provide both patient and physician with a diagnostic conclusion for the clinical picture.
|
|
| References |
1) Brazis PW. Palsies of the trochlear nerve: diagnosis and localization--recent concepts. Mayo Clin Proc 1993 May; 68(5): 501-9.
2) von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol 1986 Dec; 104(12): 1771-6.
3) Feinberg, A.S., Newman, N.J. Schwannomas in patients with isolated unilateral trochlear nerve palsy. Am J Oph 1999 Feb;127(2):183-8.
4) S. Santoreneos, A. Hanieh and R. Jorgensen, Trochlear nerve schwannomas occurring in patients without neurofibromatosis: case report and review of the literature. Neurosurg 41 (1997), pp. 282–287.
|
|