Maculopathy in a Young Person
Digital Journal of Ophthalmology 2006
Volume 12, Number 6
December 22, 2006
Volume 12, Number 6
December 22, 2006

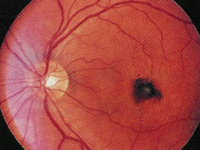
Color Fundus Photo
Fig. 1: Color fundus photograph on presentation in June 2002 shows a neurosensory detachment with gray appearance underlying it. There is a small fleck of blood temporal to center of macula.
Fig. 1: Color fundus photograph on presentation in June 2002 shows a neurosensory detachment with gray appearance underlying it. There is a small fleck of blood temporal to center of macula.
Fluorescein angiography revealed leakage under the neurosensory detachment (Figs 2 and 3).
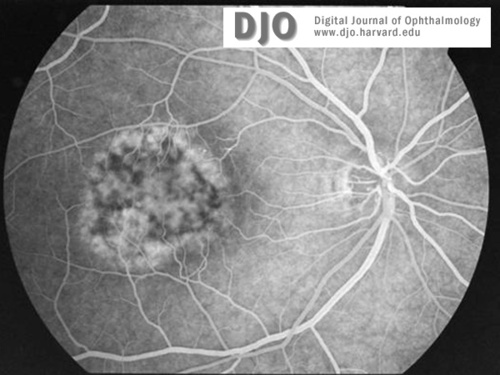
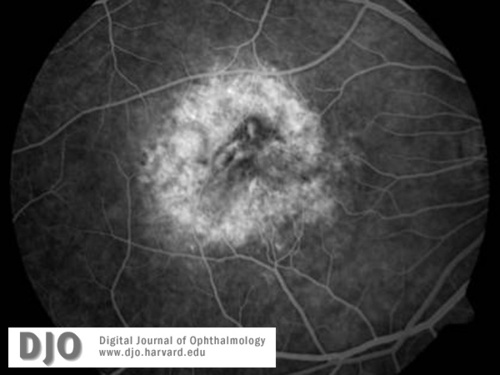
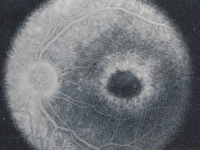
Fluorescein Angiogram
Fig. 2: Fluorescein angiogram shows leakage under the neurosensory detachment.
Fig. 2: Fluorescein angiogram shows leakage under the neurosensory detachment.
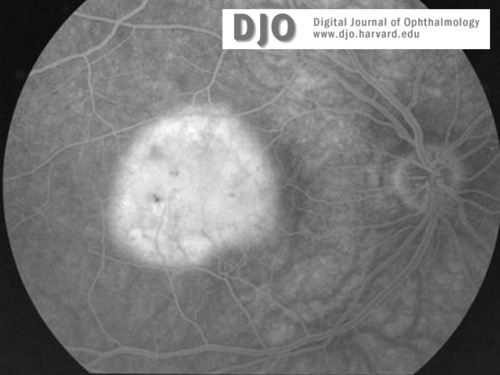
Fluorescein Angiogram
Fig. 3:Fluorescein dye fills neurosensory detachment in late phase photos. Note blocking by blood temporal to center of macula.
Fig. 3:Fluorescein dye fills neurosensory detachment in late phase photos. Note blocking by blood temporal to center of macula.
The patient’s vision subjectively improved over the next several months. No further PDT treatments were performed. Fourteen months after presentation, the patient’s acuity was 20/20 OD. There was a small stable paracentral scotoma on Amsler testing OD, which had been present for several months. There wass some evolution of the subretinal pigmentary changes which replaced the neurosensory detachment, with atrophy surrounding central hypereigmentation (Fig. 6). Fluorescein angiography showed transmission of hyperfluoresence from the large choroidal vessels early (Fig. 7). In the late images there was staining of the pigmentary atrophy with blockage from the central area of hyperpigmentation (Fig. 8).
After giving the verteporfin photodynamic therapy, we had become aware of unilateral acute idiopathic maculopathy (UAIM), first described by Yannuzzi et al (Arch Ophthalmol 1991;Vol 109;1411-1416). UAIM usually affects young adults with a loss of central vision after a flu-like illness. Patients typically present with <20/200 central vision. Examination commonly reveals a neurosensory detachment with irregular margins, white-gray subretinal thickening at the level of the RPE, and occasional intraretinal hemorrhage (Fig. 9). Some patients present with mild vitritis. In the initial series, the fellow eye was unaffected. On fluorescein angiography, progressive leakage of dye with pooling in the subretinal space was seen (Figs. 10 and 11).
The natural course of UAIM, as initially described by Yanuzzi, was gradual improvement over three months to 20/25+ in 7 of the 9 initial patients. The neurosensory detachments resolve and the central macula typically develops mild, late subretinal fibrous metaplasia with surrounding RPE hypopigmentation often resembling a “bull’s eye.” (See Fig. 12). On fluorescein angiography, the leakage pattern is replaced by staining of the atrophic areas and blocking by central pigment (Figs. 13 and 14). There were no recurrences in 2.5 to 13 years of follow-up in the initial series.
In retrospect, our patient had UAIM. Her clinical presentation and course as documented by color photography and fluorescein angiography was typical for this condition. We are glad the unnecessary Verteporfin photodynamic therapy does not seem to have adversely affected the long term outcome.

Color Fundus Photo
Fig. 4: Color fundus photography one month after presentation. Neurosensory detachment has been replaced by dry pigmentary changes.
Fig. 4: Color fundus photography one month after presentation. Neurosensory detachment has been replaced by dry pigmentary changes.
Fluorescein Angiogram
Fig. 5: Late phase photograph from fluorescein angiography one month after presentation has staining but no leakage.
Fig. 5: Late phase photograph from fluorescein angiography one month after presentation has staining but no leakage.

Color Fundus Photo
Fig. 6: Color fundus photography 14 months after presentation. There is evolution of the dry pigmented changes.
Fig. 6: Color fundus photography 14 months after presentation. There is evolution of the dry pigmented changes.
Fluorescein Angiogram
Fig. 7: Fluorescein angiography 14 months after presentation shows large choiodal vessels in areas of pigmentary atrophy.
Fig. 7: Fluorescein angiography 14 months after presentation shows large choiodal vessels in areas of pigmentary atrophy.
Fluorescein Angiogram
Fig 8: Late phase photograph 14 months after presentation shows staining in areas of atrophy and blocking by central hyperpigmentation.
Fig 8: Late phase photograph 14 months after presentation shows staining in areas of atrophy and blocking by central hyperpigmentation.

Color Fundus Photo
Fig. 9: Color fundus photography from Yanuzzi et al’s article showing typical findings of UAIM on presentation. (from Yannuzzi et al 1991, reproduced with permission)
Fig. 9: Color fundus photography from Yanuzzi et al’s article showing typical findings of UAIM on presentation. (from Yannuzzi et al 1991, reproduced with permission)
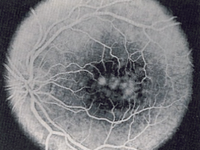
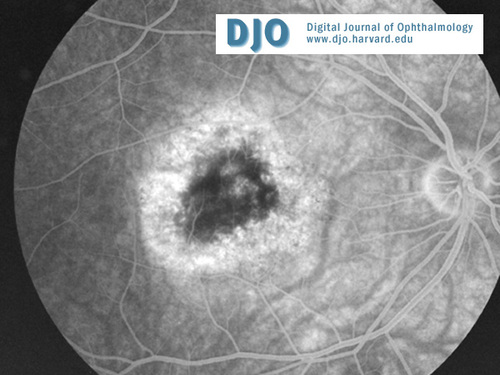
Fluorescein Angiogram
Fig. 10: Mid phase angiography of UAIM on presentation shows early leakage (Yannuzzi et al 1991; reproduced with permission)
Fig. 10: Mid phase angiography of UAIM on presentation shows early leakage (Yannuzzi et al 1991; reproduced with permission)
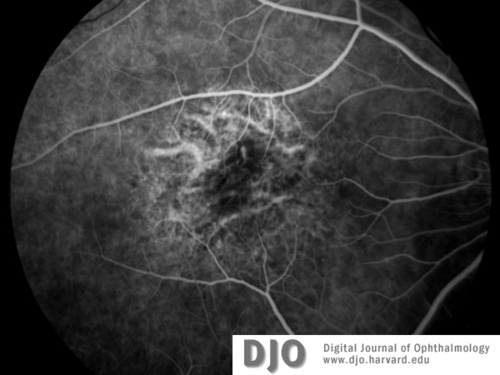
Fluorescein Angiogram
Fig 11: Late phase photograph of UAIM on presentation shows pooling of dye under neurosensory detachment. (Yanuzzi et al, 1991; reproduced with permission)
Fig 11: Late phase photograph of UAIM on presentation shows pooling of dye under neurosensory detachment. (Yanuzzi et al, 1991; reproduced with permission)
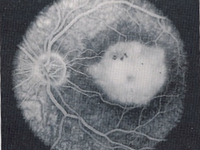
Color Fundus Photo
Fig 12: Color fundus photography from Yanuzzi et al’s 1991 article showing central subretinal fibrous metaplasia with surrounding pigment epithelial atrophy typical of later UAIM. Reproduced with permission.
Fig 12: Color fundus photography from Yanuzzi et al’s 1991 article showing central subretinal fibrous metaplasia with surrounding pigment epithelial atrophy typical of later UAIM. Reproduced with permission.
Fluorescein Angiogram
Fig. 13: Late phas fluorescein angiogram shows the leakage pattern is replaced by staining of the atrophic areas and blocking by central pigment (Yannuzzi et al 1991; reproduced with permission)
Fig. 13: Late phas fluorescein angiogram shows the leakage pattern is replaced by staining of the atrophic areas and blocking by central pigment (Yannuzzi et al 1991; reproduced with permission)
Freund KB, Yannuzzi LA, Barile GR, Spaide RF et al. The Expanding clinical spectrum of unilateral acute idiopathic maculopathy. Arch Ophthalol 1996;114:555-559.