An 89-year-old man with acute vision loss in the right eye
Digital Journal of Ophthalmology 2007
Volume 13, Number 6
February 10, 2007
Volume 13, Number 6
February 10, 2007
An eighty-nine year-old Caucasian man presented with a one week history of acute loss of vision in his right eye. The ocular history included cataract surgery bilaterally with posterior chamber intraocular lens placement twenty years ago. His past medical history included hypertension, chronic obstructive pulmonary disease, abdominal aortic aneurysm and colon cancer status post partial colectomy eight years ago. His medications were metoprolol 50 mg daily and a combivent inhaler as needed.
Because of his age, history of hypertension and systemic vasculopathy, macroaneurysm and macular degeneration were considered as likely causes of the macular bleeding. On follow up examination, his condition remained stable and pneumatic translocation of the hemorrhage was offered to the patient. Considering his good visual acuity in the left eye and fear of complication from the procedure, he declined the intervention. Two weeks later the patient returned to clinic complaining of worsening vision and pain in the right eye. The intraocular pressure in the right eye was 27 and there was an inferior hemorrhagic choroidal detachment present (Figure 1). The patient was started on intraocular pressure lowering agents and anti-inflammatory drops. Ten days later the patient returned with severe eye pain and an intraocular pressure of 64. The retina could not be viewed due to vitreous hemorrhage.
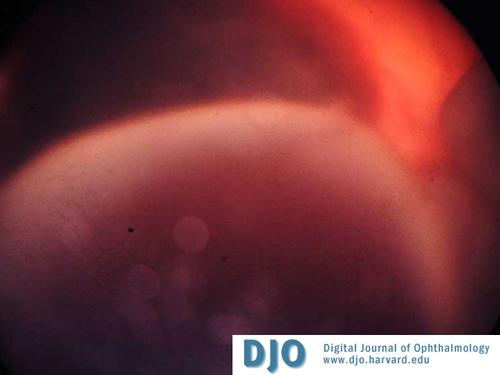
Figure 1
Right eye with inferior choroidal hemorrhage
Right eye with inferior choroidal hemorrhage

Figure 2
Extensive periorbital hemorrhage tracked subcutaneously down the right side of the patient's face
Extensive periorbital hemorrhage tracked subcutaneously down the right side of the patient's face
An ultrasound revealed kissing choroidals and four quadrants of dense choroidal hemorrhage filling the vitreous cavity of the right eye.
A DIC panel indicated an elevated D-dimer of 5373 ug/L (normal 0-500ug/L), fibrinogen of 82 mg/dL (normal 210-440mg/dL) and fibrin split products >40 ug/dL (normal 0). These laboratory values fit the criteria for DIC. The patient had a normal platelet aggregation assay. During his hospital stay he was also diagnosed with a urinary tract infection. It was postulated that the patient may have had chronic DIC from a number of his underlying medical conditions. There are reports of chronic low grade DIC associated with abdominal aortic aneurysm as well as systemic infection such as urosepsis. In this case the hematology team thought that his urinary tract infection was the cause of DIC as other diagnostic tests were negative. He was treated with vitamin K 5 mg subcutaneously for 3 days and his UTI was aggressively treated with IV antibiotics. His INR by the end of his hospital stay was 1.17. His final vision was no light perception in his right eye.
DIC is caused by the excessive generation of thrombin leading to a cascade of reactions that occur in an unregulated fashion. Thrombin activates platelets and induces platelet aggregation. It also induces the release of tissue plasminogen activator (t-PA). Plasminogen is cleaved to release plasmin resulting in fibrinolysis in the normal coagulation cascade. In DIC, the excess thrombin subsequently results in vigorous fibrinolysis by excess plasmin activity, thereby resulting in concurrent excess of thrombosis and bleeding.(3)
Case reports in the literature have described histopathological descriptions of patients with known DIC having serous retinal detachment, thrombotic occlusion of choriocapillary vessels and hemorrhage within the choroid at time of autopsy. Cogan described the histopathological effects of DIC upon the choroids.(4) Characteristic similarities among the cases include thrombosis within the smaller choroidal vessels, organization over time by hyaline formation and endothelial proliferation, and hemorrhage into the choroid but not extending through Bruch’s membrane. The thromboses within the choriocapillaris result in hemorrhage into the choroid and serous exudation into the subretinal space. Endothelial proliferation described in one case suggested neovascularization as a result of a chronic process. These findings indicate that DIC compromises the structural integrity of the choroid and results in microscopic evidence of choroidal hemorrhage. Long term follow up of the above mentioned cases was impossible as they each died from their underlying disorder. We suggest that a patient with DIC for a prolonged period of time can have microscopic signs of DIC that may progress to gross hemorrhage over time.
A few underlying disorders known to initiate DIC include sepsis, malignancy, and mechanical tissue injury. Any of these disease entities may trigger the excess production of thrombin and plasmin resulting in a consumption coagulopathy. In the patient presented, this may include urinary tract infection, history of cancer and aortic aneurysm.(5) The clinical expression of DIC may vary from fulminant to subacute or chronic. Our patient did not present with the characteristic systemic presentation of fulminant DIC. Although the presentation can be variable, he did not present with common clinical findings such as petechiae and purpura, hypotension, or frank bleeding from unrelated sites prior to the choroidal hemorrhage. Based on clinical presentation our patient was thought to have had a subacute or chronic form of DIC, also known as compensated DIC. He responded to the recommended vitamin K as evidenced by the normalization of follow up serial labs. The blood tracking down his face and neck also resolved over time following vitamin K administration. We suggest that in the presence of a spontaneous choroidal hemorrhage, even in the absence of other end organ damage, it may be advantageous to consider a bleeding diathesis such as DIC as a potential etiology of the bleeding.
2. Yang SS, Fu AD, McDonald HR, Johnson RN, Ai E, Jumper JM. Massive spontaneous choroidal hemorrhage. Retina. 2003 Apr;23(2):139-44.
3. Bick RL. Disseminated intravascular coagulation current concepts of etiology, pathophysiology, diagnosis, and treatment. Hematol Oncol Clin North Am. 2003 Feb;17(1):149-76.
4. Cogan DG. Ocular involvement in disseminated intravascular coagulopathy. Arch Ophthalmol. 1975 Jan;93(1):1-8.
5. Siebert WT, Natelson EA. Chronic consumption coagulopathy accompanying abdominal aortic aneurysm. Arch Surg. 1976 May;111(5):539-41.