A 15-year-old girl with sudden onset proptosis
Digital Journal of Ophthalmology 2006
Volume 12, Number 5
December 12, 2006
Volume 12, Number 5
December 12, 2006
Prior to the trauma, the patient had experienced episodes of intermittent prominence and ‘bulging’ of the left eye. Her mother first noticed this at the age of two years and she was taken to see a pediatric ophthalmologist. Following an orbital ultrasound, she was diagnosed with a left orbital varix. At this time, the lesion was said to consist of a low flow mass surrounding the optic nerve, which extended widely through the orbit. The patient had been asymptomatic for the last twelve years and not followed up routinely.
Given her past history, a presumed diagnosis of variceal hemorrhage was made.
Blood tests including complete blood count, CRP and ESR were unremarkable.An MRI scan of the orbits was performed to confirm the diagnosis (Figure 2).
Figure 2 MRI scan of orbits
A large left sided intraconal mass lesion is present. It is well defined and contains a number of septations. The lesion is distorting the globe and causing expansion of the orbital cavity with proptosis. The lesion returned a fluid signal on STIR and T2, with a signal slightly higher than fluid on T1. There was no enhancement following Gadolinium.
The appearance is consistent with an orbital venous malformation.
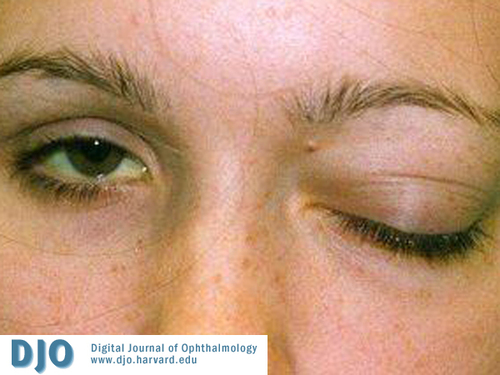
Figure 1
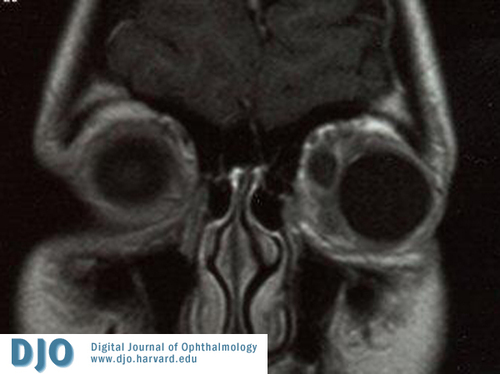
Figure 2A

Figure 2B
She was managed conservatively with careful observation of her optic nerve function. Two days following admission she had begun to improve symptomatically and cosmetically with a reduction in the proptosis.
The gradual improvement continued and she was discharged on day five. There was complete resolution of proptosis and the intraocular pressure has returned to normal.
A retrospective analysis by Sindhu et al examined 57 children with proptosis. Orbital cellulitis was the most common cause (22 cases), followed by thyroid eye disease (8), optic nerve glioma (8), orbital rhabdomyosarcoma (7), metastatic neuroblastoma (4), orbital neurofibroma (3) and orbital haemangioma (2) [3].
In this case, cellulitis was unlikely as the patient was afebrile, the skin was not warm and inflammatory markers were not raised. Thyroid eye disease does occur in children, and is well recognized in neonates of hyperthyroid mothers, however, in our patient the signs were asymmetrical, there was no lid lag and the extraocular muscles appeared normal on the MRI. The patient had no signs of neurofibromatosis, which may have suggested an associated optic nerve glioma. A lesion of the optic nerve or orbital apex was also unlikely as in these cases, visual acuity or ocular motility tend to be affected early. Finally rhabdomyosarcoma was considered in the differential diagnosis, however, given the childhood history of intermittent proptosis and clinical course following admission this was very unlikely [1].
Orbital vascular malformations (OVMs) are anomalies of blood vessels caused by errors of vasculogenesis. They may occur isolated within the orbit or in association with vascular anomalies elsewhere [4].
Until recently, there has been controversy regarding the classification of OVMs, which reflects a poor understanding of the origin of these lesions and may complicate treatment decisions. In 1999 the Orbital Society published a consensus statement on the terminology of OVMs [2]. Vascular malformations were classified as no flow malformations (e.g. lymphangiomas), arterial flow malformations (e.g. arteriovenous malformations) or venous flow malformations according to communications with the systemic vascular system. Venous flow malformations are weakened segments of the orbital venous system of variable complexity. This group is further classified as distensible (clinical or radiological evidence of distensibility with increased venous pressure), or nondistensible. Distensible lesions have direct and rich communication with the venous circulation and nondistensible lesions have a direct communication but to a much lesser extent.
Spontaneous orbital haemorrhage and thrombosis can occur in all types of vascular malformations but may be more common in nondistensible lesions, which have stagnant blood flow [5].
The largest study of orbital vascular malformations demonstrated the varied presentations of such lesions [6]. This retrospective series examined 158 patients with a diagnosis of orbital venous anomaly or lymphangioma. Patients may present acutely with symptoms including pain, sudden proptosis, nausea, vomiting, diplopia or visual deterioration. An acute presentation may occur following an episode of hemorrhage or thrombosis within the lesion. OVMs may also present with intermittent proptosis as distensible lesions may expand during episodes of coughing, bending, or straining. OVMs with a superficial component may produce swelling and disfigurement of the eyelids or conjunctiva. Most patients have normal vision at presentation [7].
In Wright’s series, 55% of patients had at least one orbital hemorrhage and although this could occur at any age it was more common in patients less than 30 years of age. Bleeding into surrounding tissues was frequent often resulting in bruising of the eyelids and subconjunctival tissues. Compression of the optic nerve was uncommon and in most cases vision was not permanently impaired.
Orbital CT with contrast or MRI, are reliable ways of demonstrating OVMs. CT typically shows a smooth, rounded homogenous mass denser than brain. However, OVMs can produce variable appearances depending on the flow and the evolutional stage of any haemorrhage or thrombosis within the lesion.
This case raises important questions regarding the natural history of orbital venous anomalies. The lesion in this case had remained quiescent for more than ten years, only to re-present acutely following minor trauma. OVMs tend to enlarge either at haemorrhagic intervals or progressively without haemorrhage. Interestingly the incidence of haemorrhage decreases in later life. This suggests that malformations achieve stability perhaps secondary to fibrosis.
Patients should be treated as conservatively as possible. OVMs are difficult to remove surgically due to close associations with normal orbital structures and associated orbital wall defects [8]. There is also a risk of visual loss secondary to haemorrhage or optic nerve damage secondary to vascular compromise [9].
If intervention is indicated, the least invasive method should be employed first as these lesions are benign and symptomatic treatment will usually suffice. Indications for intervention may include severe pain, hemorrhage causing severe proptosis or optic nerve compression, or a well circumscribed lesion causing a cosmetic defect or significant proptosis. Surgical options include evacuation of haemorrhage, excision, carbon dioxide laser ablation, embolisation with platinum Guglielmi detachable coils and percutaneous alcohol sclerotherapy.
1. Taylor D, Hoyt C. Pediatric Ophthalmology and Strabismus. Elsevier Saunders. Third Edition 2005.
2. American Academy of Ophthalmology. Basic and Clinical Science Course. Pediatric Ophthalmology and Strabismus. Section 6 2002-2003.
3. Sindhu K, Downie J, Ghabrial R, et al. Aetiology of childhood proptosis. Journal of Paediatrics and Child Health 1998; 34:374-376.
4. Lacey B, Rootman J. Distensible venous malformations of the orbit: clinical and hemodynaimc features and a new technique of management. Ophthalmology 1999; 106:1197-209.
5. Harris GJ. Orbital vascular malformations: a consensus statement on terminology and its clinical implications. Am J Ophthalmology 1999; 127:453-455.
6. Arat YO, Mawad ME, Boniuk M. Orbital venous malformations. Arch Ophth 2004; 122:1151-1158.
7. Wright JE, Sullivan TJ, Garner A, Wulc AE, Moseley IF. Orbital venous anomalies. Ophth 1997; 104:905-913.
8. Islam N, Mireskandari K, Rose GE. Orbital varices and orbital wall defects. Br J Ophthalmology 2004; 88:1092-1103.
9. Harris GJ, Sakol PJ, Bonavolonta G, et al. An analysis of thirty cases of orbital lymphangioma. Pathophysiologic considerations and management recommendations. Ophthalmology 1990; 97:1583-92.