A 63 year-old woman with enophthalmos
Digital Journal of Ophthalmology 2005
Volume 11, Number 12
July 10, 2005
Volume 11, Number 12
July 10, 2005
The patient’s postoperative course after the left orbital decompression was peculiar in that she developed marked degree of enophthalmos and hypoglobus, OS, occurring subacutely post-operative. The Hertel exophthalmometry and hypoglobus measurements are presented below:
Preop: OD /OS
10/26/2000 25.5mm /25mm
Postop:
11/16/2000 23mm /20mm
12/06/2000 23mm /18mm
02/19/2000 22mm /18mm
03/22/2001 21mm /18mm 2-3mm hypoglobus OS
06/04/2001 19mm /14mm
04/15/2002 18mm /15mm 2mm hypoglobus OS
05/07/2003 18.5mm /15mm 3mm hypoglobus OS
Past Ocular history:
1. Severe Graves orbitopathy, OU; severe thyroid optic neuropathy, OS; mild thyroid optic neuropathy, OD.
2. Transconjunctival orbital floor and medial wall decompression with preservation of maxillo-ethmoidal strut, OS. 11/2/2000; s/p similar right orbital decompression on 2/13/2001.
3. Status post left medial rectus recession 4-5 mm and left inferior rectus recession 3.5 mm with Spielmann technique in 11/2001 for left esotropia and hypotropia.
Past medical History: Graves disease
Medications: none
Social History: materials clerk. Married, three children. 40-pack-year history of smoking
Family History: significant for autoimmune disease on father’s side. A paternal grandfather with a goiter, father with diabetes and a sister with alopecia.
Vision: OD: 20/20, OS 20/30-2
Pupils: normal
External Exam:
Hertel exophthalmometry (base 92): OD 18mm, OS 14mm.
Hypoglobus: 4mm OS
Superior Sulcus defect, OS
Motility:
full OD; -1 to temporal, superior temporal, superior nasal, and upward movements OS
Slit lamp examination: unremarkable
Figure 1. Exophthalmos before left orbital decompression (10/26/2000)
Figure 2. Hypoglobus (01/24/2001, two and a half months post-op)
Figure 3. a. Hypoglobus (10/15/2001, 11 months after the surgery). b. Marked degree of enophthalmos (10/15/2001, 11 months after the surgery)

Figure 1.
Exophthalmos before left orbital decompression (10/26/2000).
Exophthalmos before left orbital decompression (10/26/2000).

Figure 2.
Hypoglobus (01/24/2001, two and a half months post-op).
Hypoglobus (01/24/2001, two and a half months post-op).
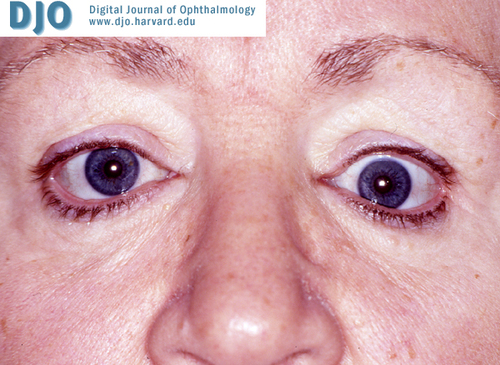
Figure 3a.
Hypoglobus (10/15/2001, 11 months after the surgery).
Hypoglobus (10/15/2001, 11 months after the surgery).
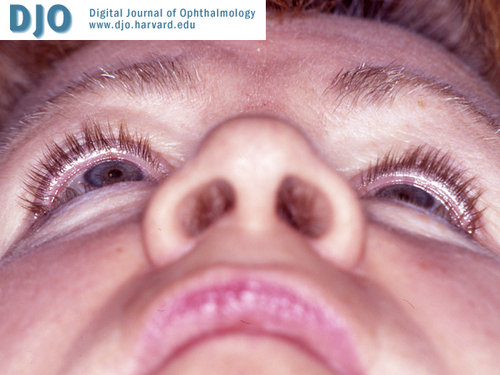
Figure 3b.
Marked degree of enophthalmos (10/15/2001, 11 months after the surgery).
Marked degree of enophthalmos (10/15/2001, 11 months after the surgery).
Radiology
Figure 4. a. Coronal computed tomography scan (05/28/2003) shows complete obliteration of the left maxillary infundibulum and downward prolapse of the orbital contents, with secondary hypoglobus. Note the right ethmoidal infundibulum of the maxillary sinus (arrow). There is near complete opacification of the left maxillary sinus. b. There is inward bowing (implosion) of the lateral wall of the left maxillary sinus. Also note bilateral extraocular muscle hypertrophy, predominantly involving the superior, medial and inferior rectus muscles.
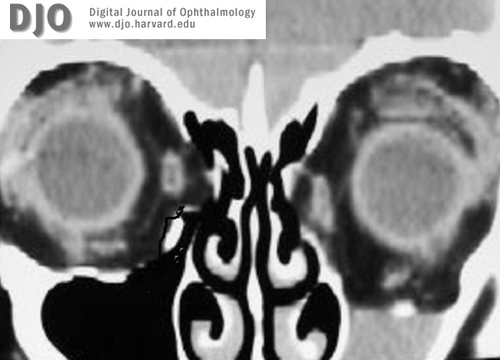
Figure 4a.
Figure 4. a. Coronal computed tomography scan (05/28/2003) shows complete obliteration of the left maxillary infundibulum and downward prolapse of the orbital contents, with secondary hypoglobus. Note the right ethmoidal infundibulum of the maxillary sinus (arrow). There is near complete opacification of the left maxillary sinus.
Figure 4. a. Coronal computed tomography scan (05/28/2003) shows complete obliteration of the left maxillary infundibulum and downward prolapse of the orbital contents, with secondary hypoglobus. Note the right ethmoidal infundibulum of the maxillary sinus (arrow). There is near complete opacification of the left maxillary sinus.
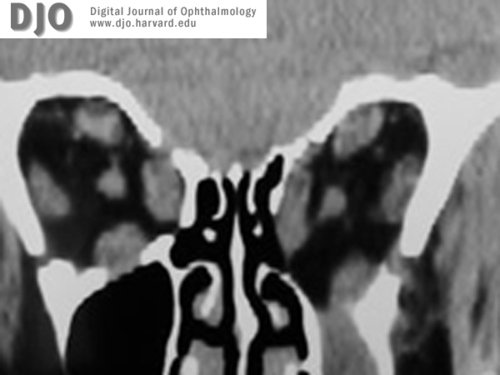
Figure 4b.
There is inward bowing (implosion) of the lateral wall of the left maxillary sinus. Also note bilateral extraocular muscle hypertrophy, predominantly involving the superior, medial and inferior rectus muscles.
There is inward bowing (implosion) of the lateral wall of the left maxillary sinus. Also note bilateral extraocular muscle hypertrophy, predominantly involving the superior, medial and inferior rectus muscles.
Rose et al (2) applied the term “imploding antrum syndrome” to describe 14 patients with mean age of 41 years who presented with the very characteristic clinical features similar to those reported by Soparkar et al (1). They reported average enophthalmos being 2.8 mm compared with 3.0 mm in the Soparkar series, and a mean hypoglobus of 2.2 mm compared with 3.4 mm. The concavity of maxilla walls including medial, posterolateral, and/or anterior was universally present, with anterior walls absent in 2 of 14 patients. However, this series showed various changes in the maxillary walls—with thickening, generalized thinning, or focal loss of bone. This study also demonstrated that, in 10 of 14 patients, nasal septal deviation occurred toward the involved side. This contrasted to Soparker and Patrinely’s (5) updated series in which only 32% of patients had deviations towards the affected side. There were abnormalities of the ipsilateral middle turbinate and osteomeatal complex. Interestingly, where the posterolateral maxillary wall was affected, there was a concomitant increase in the fat content in the pterygopalatine fossa. They preferred the term “imploding antrum syndrome” to “silent sinus syndrome”.
Rose et al (3) recently proposed a hypothesis to explain the underlying pathophysiology for iatrogenic and idiopathic “imploding antrum” (silent sinus) syndrome. They described features and treatment of late enophthalmos in six patients who underwent three-wall orbital decompression for thyroid eye disease. All six patients had a satisfactory degree of decompression in the early postoperative period. However, over a few months after surgery, they experienced enophthalmos and hypoglobus. Two patients had a clear history of ipsilateral sinusitis shortly before the onset of enophthalmos. Radiologically, 5 of 6 patients displayed inward bowing of the posterolateral antral wall. There was occlusion of the ethmoidal infundibulum by prolapsed orbital fat, with secondary opacification of the maxillary antrum in all six patients. In the unaffected maxillary antrum of all 6 patients, aeration was present, and the unoperated walls were normal. When the maxillary-ethmoidal interface was intact, the ethmoidal infundibulum was found to be patent with normal maxillary antral aeration. When there was prolapse of orbital fat into the ethmoidal infundibulum obstructing aeration of the maxillary antrum, drainage of sinus secretions into the middle meatus was blocked, and the opacification of the sinus ensued. With ongoing resorption of antral fluid, pressure in the sinus might become sub-atmospheric, resulting in downward movement of the orbital floor producing secondary enophthalmos and hypoglobus. Inferior soft tissue prolapse further blocks antral drainage and worsens aeration. The impact of the long-standing subatmospheric pressure within the maxillary sinus may lead to implosion of the other walls of the sinus. This process may eventually stabilize when the antral walls have undergone maximal remodeling.
During orbital decompression, it is critical to retain the maxillo-ethmoidal interface (inferomedial bone strut). Retaining the maxillo-ethmoidal strut also helps prevent large inferomedial displacement of the globe following orbital decompression. In the event that the bone strut is removed, medial antrostomy should be considered.
2. Rose GE, Sandy C, Hallberg L et al. Clinical and radiologic characteristics of the imploding antrum, or “silent sinus,” syndrome. Ophthalmology 2003; 110:811-818.
3. Rose GE, Lund VJ. Clinical features and treatment of late enophthalmos after orbital decompression. Ophthalmology 2003; 110:819-826.
4. Davidson JK, Soparker CNS, Williams JB, Patrinely JR. Negative sinus pressure and normal predisease imaging in silent sinus syndrome. Arch Ophthalmology 1999; 117:1653-1654.
5. Soparker CNS, Patrinely JR, Davidson JK. Silent sinus syndrome – new perspectives? Ophthalmology 2004;111:414-415.
