A 65 year old woman with visual changes
Digital Journal of Ophthalmology 2005
Volume 11, Number 14
July 28, 2005
Volume 11, Number 14
July 28, 2005
Uveal metastasis has been shown to be the most common form of intraocular malignancy. Over 85% of metastatic uveal neoplasms are choroidal. Most of these metastases to the eye are carcinomas, originating mostly from breast and lungs cancers, although primary neoplasms from several other tissues have been reported. Carcinoid metastatic to the choroid is rare; it is reported to comprise slightly more than 2% of uveal metastases. The following is the presentation of a case of carcinoid metastatic to the choroid and its response to our treatment.
History
A 65-year-old woman presented complaining of 6 weeks of “seeing blobs of silver light” in her left eye lasting 2-3 seconds per episode. The patient’s ocular history was significant for moderate myopia. Her medical history was remarkable for carcinoid metastatic to her liver and pancreas, as well as hypercholesterolemia and high blood pressure.
The patient’s carcinoid tumor presented as a cough over six years ago, and was definitively diagnosed by bronchial biopsy with histopathology one year after presentation. Systemic work-up at that time was negative; the patient had no symptoms of carcinoid syndrome and had a laboratory profile, including a 5-HIAA level, within normal limits. An MRI of the brain was normal. The bronchial carcinoid was treated with short-term chemotherapy followed by radiation therapy to the primary lesion with a good response following 50.4 Gy of radiation therapy. The patient eventually developed metastases to both her liver and pancreas. Her carcinoid is followed by her oncologist and treated with sandostatin 20mg once a month.
On ophthalmic examination, the patient’s visual acuity with corrective lenses was 20/40 OU and did not improve with pinhole. She had full visual fields, full, orthotropic extraocular muscle movement and no afferent papillary defect. Intraocular pressures were normal. Anterior segment examination was normal except for trace nuclear sclerosis OU. Fundus exam of the right eye was unremarkable. Fundus exam of the left eye revealed a supranasal tumor 4 disc diameters x 4 disc diameters in area with an orange pigmentation (Figure 1).
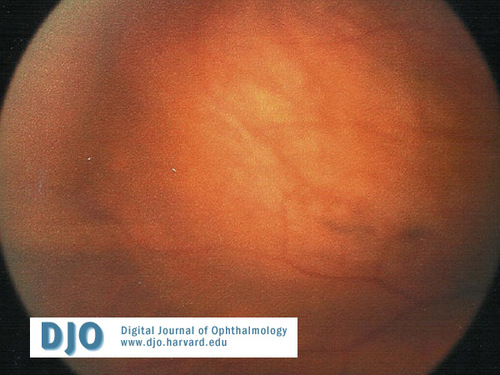
Color Photograph
Color fundus photo of the lesion
Color fundus photo of the lesion
Ancillary Testing
A fluorescein angiogram performed at the initial visit was remarkable for mottled hyperfluorescence in the early venous phase (Figures 2 and 3). Ultrasonographic data revealed a largely homogenous mass with a medium to low internal reflectivity, and a strong initial and scleral spike. No internal quiet zone was noted. Dimensions on were noted to be 14.54mm x 13.86mm x 4.45-4.7mm (Figure 4). An MRI of the brain with and without contrast revealed a plaque-like, lenticular-shaped, homogeneously enhancing retinal-based mass in the superomedial portion of the left globe. The lesion was isointense to the brain on both T1- and T2-weighted images.
Early Phase Angiogram
Angiogram of the mass at 0:08
Angiogram of the mass at 0:08
Peak Phase Angiogram
Angiogram of the mass at 0:34
Angiogram of the mass at 0:34
Pre-Radiation Ultrasound
L930 B-scan of the mass before external beam radiation
L930 B-scan of the mass before external beam radiation
Post-Radiation Ultrasound
L930 B-scan of the mass after external beam radiation
L930 B-scan of the mass after external beam radiation
The decision was made for the patient to undergo external palliative radiotherapy for carcinoid disease with presumed metastasic to the left choroid. The patient was scheduled to receive 41.4 Gy of radiotherapy over 23 daily fractions. On follow-up examination two weeks after the start of treatment, the patient’s visual acuity was 25-1 OD and 25-2 OS with correction. Following treatment, the tumor had notably decreased in size on fundus examination and photography. Ultrasonography at that time confirmed decreased tumor mass with dimensions of 9mm x 10.5mm x 2.9mm (Figure 5). Ultrasound changes included a slightly lower internal reflectivity. Additionally, repeated fluorescein angiogram also revealed a significantly smaller tumor with mottled hyperfluorescence in the early venous phase.
The physical appearance of the tumor on exam includes any amelanotic, orange mass in the differential, including choroidal hemangioma, choroidal osteoma, exophytic retinal capillary hemangioma, other metastatic carcinomas, posterior scleritis, hemorrhagic retinal pigment epithelium detachment, and amelanotic choroidal melanoma.
“Carcinoid” is a term used to describe any type of tumor arising from the diffuse neuroendocrine cells of the amine precursor uptake and decarboxylation system, and it comprises less than 1% of all pulmonary and colorectal cancers . It is typically slow to metastasize and is of relatively low malignant potential .
The presenting symptom in our patient was new photopsias. Although the most common presentation in choroidal metastases is painless loss of vision, several other presenting complaints including floaters, field defects, and ocular pain have been documented5. The appearance of the tumor, a dome-shaped mass with an orange color, was characteristic for carcinoid. This color is unique in contrast to the creamy-yellow hue found in most uveal metastases7. The lesion was a solitary monocular metastasis, the most typical presentation of metastatic choroidal carcinoid.
Our diagnosis of metastatic carcinoid was made without a choroidal biopsy. In cases where the clinical appearance of the intraocular tumor, ultrasonography, fluorescein angiography, and a history of histopathologically confirmed systemic carcinoid tumor are strongly suggestive of the diagnosis, biopsy has been obviated7. In addition, our work-up of the patient revealed the characteristic, yet non-specific fluorescein angiography pattern typical for metastases , which is prominent hyperfluoresence in late phases of the angiogram, consistent with the prominent vascularity of metastases. Ultrasonographic findings of intermediate reflectivity were consistent with metastatic neoplasms .
In a recent review of reported cases of carcinoid metastatic to the uvea, Fan and associates found that the bronchus was the site of the primary tumor in 24 of 28 cases. Although the gastrointestinal tract is the location for over 90% of carcinoid tumors diagnosed, those that metastasize to the choroid are most frequently found in the bronchus7,8, whereas gastrointestinal carcinoid tumors most frequently metastasize to the orbit . The interval between detection of the primary carcinoid and the diagnosis of uveal metastases has been reported as being between 0 and 9 years with an average of 4.1 years .
Treatment for metastatic choroidal carcinoid has not been standardized. Due to the rarity of this diagnosis and the interval between the detection of new cases, a powerful prospective therapeutic trial would be very difficult to produce. For decades, the most commonly employed therapy for patients with systemic malignancies metastatic to the choroid has been external beam radiation therapy, ranging between 20Gy to 50Gy fractionated , , . The assumption that radiation would effectively treat ocular carcinoid may be flawed, however, since external beam radiation has incomplete success for primary carcinoid tumors , . Despite the literature that carcinoid tumors are generally radioresistant, there are reports from groups that have observed these tumors effectively treated by both external beam radiation and plaque brachytherapy7, . There is an equal paucity of information regarding metastatic ocular carcinoid response to chemotherapy; however, there is one case report of cisplatin and etoposide being effective treatment . Our patient had a remarkably good response to external beam radiation treatment of her primary bronchogenic carcinoid. This result early in her initial course suggested that she would achieve the observed, good response of her choroidal lesion following palliative radiation. Although radiation treatment of carcinoid metastatic to the choroid has mixed results in the literature, we are encouraged by our patient’s tumor reduction after treatment.
Early detection and treatment of ocular carcinoid is important due to the comparatively favorable prognosis of patients with carcinoid metastatic to the choroid. Orbital and intraocular metastases are generally associated with a grave prognosis, and the interval between surgical intervention and death is usually measured in months4. However, there are several cases of choroidal carcinoid with prolonged survival, and the prognosis for patients with this rare choroidal metastasis can be measured in years. The indolent course of systemic carcinoid and extended survival observed in some cases of ocular carcinoid justify aggressive intervention to improve prognosis. Harbour et al has observed a mean survival of 34 months from ocular diagnosis7, and Fan et al observed 4 study patients surviving over 7 years after choroidal metastases were diagnosed . Such encouraging reports, the documented radioresponsiveness of our patient’s specific tumor, and the rapid and remarkable response of the ocular metastasis we have observed allow us an above-average prognosis in this case.
Nelson CC, Hertzburg BS, Klintworth GK. A histopathalogic study of 716 unselected eyes in patients with cancer at the time of death. Am J Ophthalmol 1983; 95:788-93.
Bloch RS, Gartner S: The incidence of ocular metastatic carcinoma. Arch Ophthalmol 1971; 85:673-675.
Ferry AP, Font RL: Carcinoma metastatic to the eye and orbit: I. A clinicopathological study of 227 cases. Arch Ophthalmol 1974; 92:276-286.
Shields JA, Shields CL, Gross NE, et al: Survey of 520 eyes with uveal metastases. Ophthalmology 1997; 104:1265-1276.
Castro PA, Albert DM, Wang WJ: Tumors metastatic to the eye and adnexa. Int Ophthalmol Clin 1982; 22:189-223.
Harbour, JW, Potter, PD, Shields, CL, Shields, JA: Uveal metastasis from carcinoid tumor. Ophthalmology 1994; 101:1084-1090.
Goodwin JD II. Carcinoid tumors. An analysis of 2,837 cases. 1975; Cancer 36:560-9.
Norton JA, Lewis B, Jensen RT. Carcinoid tumors. In: DeVita VT Jr, HellmanS, Rosenberg SA, editors. Principles and practice of oncology. Philadelphia: JB lippincott, 1993;1371-86.
Gombos DS, O’Brien JM: Ocular oncology: management of systemic malignancies metastatic to the eye and orbit. Ophthal Clin of No Amer 1999; 12:225-234.
Coleman DJ, Abramson DH, Jack RL: Ultrasonic diagnosis of tumors of the choroid. Arch Ophthalmol 1974; 91:344-354.
Shields CL, Shields JA, Eagle, RC Jr. Orbital metastases from a carcinoid tumor. Computed tomography, magnetic resonance imaging, and electron microscopic findings. Arch Ophthalmol 1983; 101:1395-8.
Riddle PJ, Font RL, Zimmerman LE. Carcinoid tumor of the eye and orbit: a clinicopathologic study of 15 cases with histochemical and electron microscopic observations. Hum Pathol 1982; 13:459-469.
Dobrowsky W: Treatment of choroidal metastases. Br J Radiol 1988; 61:140-142.
Orenstein M, Anderson D, Stein J: Choroidal metastases. Cancer 1972; 29:1101-1107.
Reddy S, Saxena VS, Hendrickson F, et al: Malignant metastatic disease of the eye: Management of an uncommon complication. Cancer 1981; 47:810-812.
Martin RG. Management of carcinoid tumors. Cancer 1970; 26:547-51.
Schupak KD, Wallner KE. The role of radiation therapy ion the treatment of locally unresectable or metastatic carcinoid tumors. Int J Radiat Oncol Biol Phys 1991; 20:489-95.
Walker C. Bilateral choroidal metastases from “adenoma” of the bronchus. Br J Ophtalmol 1974; 58:625-9.
Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin: evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer 1991; 68:227-32.
Fan, JT, Buettner, H, Bartley, GB, Bolling, JP: Clinical features and treatment of seven patients with carcinoid tumor metastatic to the eye and orbit. Am J Ophthalmol 1995; 119:211-218.