A 79 year old man with visual changes
Digital Journal of Ophthalmology 2005
Volume 11, Number 9
April 7, 2005
Volume 11, Number 9
April 7, 2005
The visual acuity OD had been count fingers for the previous 10 years secondary to a presumed branch retinal vein occlusion. He had a history of mild cataracts OU. He was diabetic but there was no history of diabetic retinopathy or other ocular disease.
The patient had originally reported to his primary care physician one week earlier with complaints of increased fatigue, short-term memory loss, lower extremity weakness, and headache. He had been hunting in the Florida panhandle one week prior to the onset of his symptoms and sustained numerous mosquito bites.
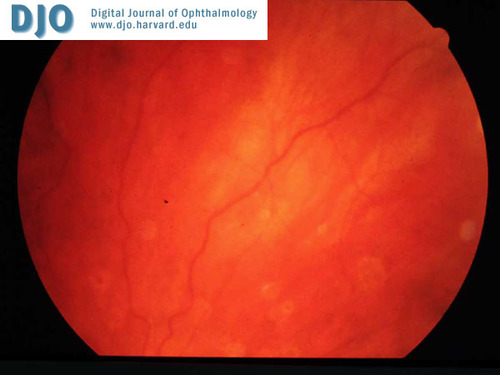
Figure 1.

Figure 2.

Figure 3.
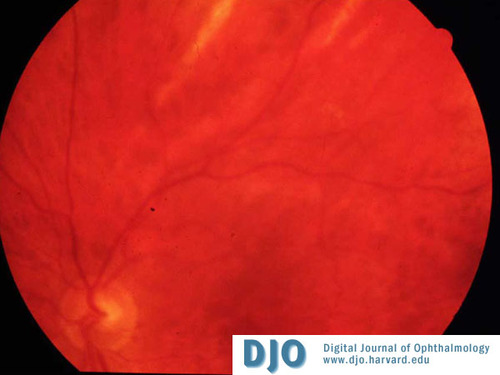
Figure 4.
A Humphrey 24-2 visual field OS showed nonspecific defects.
The patient was hospitalized and a thorough workup was initiated. CT of the head revealed no masses or acute intracranial process. A lumbar puncture was performed. The opening pressure was normal. CSF demonstrated an elevated total protein and white blood cell count; gram stain and culture were negative. Serum titers of IgG and IgM for West Nile virus were positive
Infection is usually asymptomatic but in approximately 20% of the people infected, symptoms can develop including fever, headache, fatigue, myalgias, and occasionally a skin rash on the trunk of the body. Severe infection can cause a meningitis or encephalitis picture. (2) Ocular symptoms usually begin shortly after systemic symptoms. Vision usually returns to baseline within weeks. There is no known effective treatment for systemic or ocular disease.
While the infectious etiology had been identified prior to this patient’s presentation, it is likely many patients go undiagnosed. West Nile associated choroiditis is a potential complication of viral infection that can aid in the recognition of this condition.
The ophthalmic findings in this case were consistent with several previously described cases of West Nile choroiditis. (3-7). Similar bilateral, chorioretinal, variable-sized lesions have been described in several of these reports. Findings of bilateral targetoid lesions (i.e.: hyperpigmentation surrounded by hypopigmentation) and linear hypopigmented streaks appear to be characteristic. Circular lesions range from 300-1000 microns in size and can slowly enlarge. The streak chorioretinal lesions range from 200-1500 microns in size and begin cream colored and become hypopigmented. (8) Targetoid lesions appear to be the resolving stage of initially cream-colored circular lesions, which will eventually atrophy.
Other case reports have described additional signs of West Nile ocular involvement include conjunctival hyperemia, non-granulomatous keratic precipitates, anterior chamber reaction, and occlusive retinal vasculitis, which were not found in this patient. There was no overlying retinitis, vasculitis or neurosensory detachment. It has been reported that elderly and diabetic patients are more prone to the neurologic sequelae of West Nile virus infections. (9)
This patient presented with a documented case of West Nile virus infection that made the diagnosis of coincident West Nile virus choroiditis evident. However, it demonstrates the need to include such infection in the differential diagnosis of choroiditis
2. Center for Disease Control and Prevention (CDC), Division of Vector-Borne Infectious Diseases, Questions and Answers. (2003). Available online: http://www.cdc.gov/ncidod/dvbid/westnile/qa/symptoms.htm
3. Adelman R, Membreno J, et al. West Nile Virus Chorioretinitis. The Journal of Retinal and Vitreous Diseases 2003; 23: 100-101.
4. Vandenbelt S, Shaikh S, et al. Multifocal Choroiditis Associated With West Nile Virus Encephalitis. The Journal of Retinal and Vitreous Diseases 2003; 23: 97-99.
5. Hershberger, Augsburger, et al. Chorioretinal Lesions in Nonfatal Cases of West Nile Virus Infection. American Academy of Ophthalmology 2003; 1732-1736.
6. Law S, Syed J, Caprioli J, Uveits Associated with West Nile Virus Infection. Archives of Ophthalmology 2003; 121: 1648-1647.
7. Anninger W, Lomeo M, et al. West Nile Virus-associated Optic Neuritis and Chorioretinitis. American Journal of Ophthalmology 2003; Vol 136, No 6: (1183-1185).
8. Adelman R, Membreno J, et al. Clinical Findings of West Nile Chorioretinitis. Presented at the American Academy of Ophthalmology, Retina Subspecialist meeting, 2004.
9. Chan C, Tarasewicz D, et al. Epidemiological Trends and Ocular Findings Associated with West Nile Virus Infections in North America. Presented at the American Academy of Ophthalmology, Retina Subspecialist meeting, 2004.
