A 90 year old woman with painless vision loss
Digital Journal of Ophthalmology 2005
Volume 11, Number 7
February 10, 2005
Volume 11, Number 7
February 10, 2005
ESR on initial presentation was 37mm/hr.
Hemoglobin was 13.5 and platelets were 432.
A diagnosis of anterior ischemic optic neuropathy (AION) was made. Although the clinical features were not typical of giant cell arteritis (GCA), in view of the marked visual loss in the left eye this possibility was reconsidered after 48 hours.
Repeat ESR after 48 hours was 53mm/hr and CRP was 84mg/L.
Marked patchy choroidal ischaemia and leakage at the left optic disc was noted on fundus flourescein angiography (Fig I).
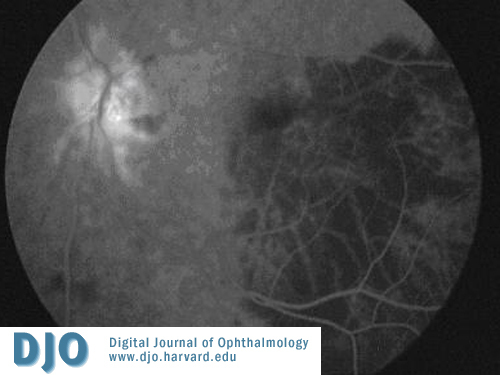
Figure 1
Temporal artery biopsy was performed and showed infiltration of the tunica adeventitia with chronic inflammtory infiltrate including giant cells (Fig 2), confirming the diagnosis of giant cell arteritis.
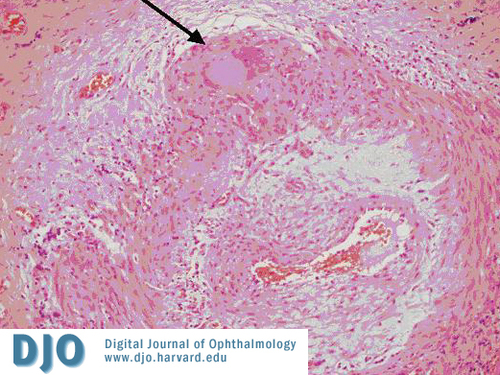
Figure 2
Arrow points to giant cell.
Arrow points to giant cell.
Anterior ischemic optic neuropathy non-arteritic type.
Optic neuritis.
Optic nerve head infiltration (infectious/non infectious/neoplastic).
i. Transient visual obscurations and/or early marked visual loss;
ii. Elevated ESR and C-reactive protein;
iii. Chalky white disc oedema and/or cilioretinal and posterior ciliary artery occlusion on flourescein angiogram; and
iv. Histological findings of arteritis.
None of the above criteria has 100% reliability. Normal ESR does not exclude giant cell arteritis. C-reactive protein is more reliable than ESR. The combination of both gives the best specificity (97%) for the diagnosis of this condition. (3, 6-8)
The most common ocular complication of GCA is ischemic optic neuropathy secondary to ischemia of the ciliary arteries. Other complications may include central retinal artery occlusion and posterior ischemic optic neuropathy. In the initial stages when the disc is edematous, the AION nerve appears chaly-white; within 6-8 weeks, atrophy develops and most patients show a pale and cupped disc. (8,9).
In the absence of systemic features of giant cell arteritis it becomes difficult to make a diagnosis of anterior ischaemic optic neuropathy of arteritic type, as was the case in our patient. She woke up with marked painless visual loss without any systemic feature of this condition. Initial ESR was also normal for her age. Repeat ESR and raised CRP raised the suspicion of GCA and it was confirmed subsequently on histology. When treated with systemic steroids the life expectancy for patients with GCA is virtually the same as for the general population. This illustrates the extreme importance of early diagnosis and treatment of GCA. (10)
Therefore, we emphasize that C-reactive protein should be requested along with ESR to enhance the specificity of the diagnosis in any patient aged more than fifty years presenting with sudden visual loss. The fundus flourescein angiogram and temporal artery biopsy should be considered in suspected cases of giant cell arteritis.
2. Simons RJ, Cogan DG. Occult temporal arteritis. Arch Ophthalmol 1962; 68:39-45.
3. Hayreh SS, Podhajsky PA, and Zimmerman B. Occult giant cell arteritis" ocular manifestations. AJO 1998;125:521-6.
4. Liu NH, LaBree LD, Feldon SE, et al. The epidemiology of giant cell arteritis: A 12 year retrospective study. Ophthalmology 2001; 108:1145-1149.
5. Gurwood AS and Malloy KA. Giant cell arteritis. Clin Exp Op. 2003;85:19-26.
6. Hayreh SS, Podhajsky PA, Raman R et al. Giant cell arteritis: Validity and reliability of various diagnostic criteria. Am J Ophthalmol 1997;123:285-296.
7. Zweegman S, Makkink, Stehouwer C.D.A. giant –cell arteritis with normal erythrocyte sedimentation rate: Case report and review of the literarture 1993;42: 128-131.
8. Hayreh SS. Acute ischemic disorders of the optic nerve: pathogenesis, clinical manifestations and management. Ophthalmol Clin North Am 1996;9:407-442.
9. Danesh-Meyer HV, Savino PJ, and Sergott RC. The prevalence of cupping in end-stage arteritic and non-arteritic anterior ischemic optic neuropathy. Ophthalmol 2001;108:593-8.
10. Matteson EL et al. Long term survival with giant cell arteritis in the American Collge of Rheumatology Giant Cell Arteritis Classification Criteria Cohort. Am J Med 1996;100:193-6.