A 24 year old woman with vision loss
Digital Journal of Ophthalmology 2004
Volume 10, Number 10
October 16, 2004
Volume 10, Number 10
October 16, 2004
- no RAPD
- anterior segments normal
- fundoscopy: right fundus oedematous, with thin vessels supero-temporally.
The initial diagnosis was a branch retinal artery occlusion and the patient was advised to stop the contraceptive pill. The following day, the patient re-presented with blurred vision, and was advised to start taking aspirin 150mg qd.
At 1 week her vision had improved to 6/6 OD and 6/5 OS.
Four days later, the patient again presented with visual loss in the right eye. the acuity was 6/12 OD. Colour plates were 10/13 OD and 11/13 OS. Fundoscopy revealed a plaque, supero-temporally. She complained of parasthaesia in right upper and lower limb.
After a week, her condition deteriorated, with of episodes of paraesthesia on the right side and slow speech lasting 30minutes, occuring 3-4 times a day. She was drowsy, had memory loss and appeared vague to her parents. Hearing was unaffected.
Blood tests revealed ESR of 47mm, fibrinogen 4.6 and CRP 15.
MRI showed mild encephalopathy and lesions in the corpus callosum, consistent with demyelination.
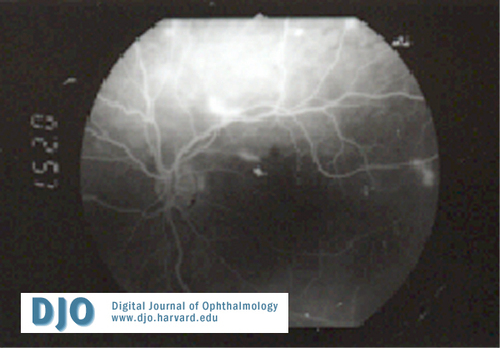
Angiography
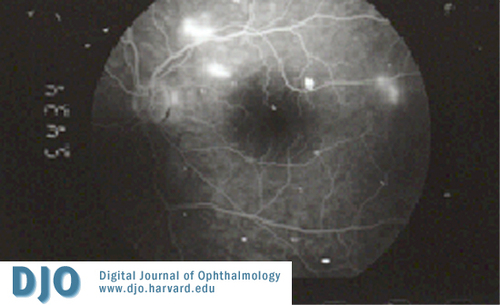
Angiography
Branch retinal artery occlusions occur, which are invariably bilateral, often as the presenting sign. Posterior pole disease causes visual loss. ESR is often elevated in these patients.
Encephalopathy, which can be subacute, seizures and myoclonus occurs. Encephalopathy may manifest as personality change, bizarre behaviour and paranoia. Bilateral extensor plantar reflexes and pseudobulbar speech patterns are noted.
Hearing loss often occurs associated with tinnitus. Microinfarction of the cochlea causes low to moderate frequency hearing loss. Microinfarction of the labyrinth causes jerk nystagmus.
EEG shows a slow pattern in encephalopathy, and MRI (imaging study of choice) shows multiple infarcts in white and grey matter. CSF protein is elavated on lumbar puncture.
Treatment may consist of intravenous immunoglbulins, steroids, plasma exchange, cyclophosphamide, and hyperbaric oxygen depending on the severity of the symptoms.
2. Susac J O, Susac's syndrome: the triad of microangiopathy of the brain and retina with hearing loss in young women. Neurology. 1994 Apr;44(4):591-3
3. Gross M, Elishar R, Banin E, Susac syndrome. Otol Neurotol. 2004 Jul;25(4):470-3.
4. Do T H, Fisch C, Evoy F, Susac syndrome: report of four cases and review of the literature. AJNR Am J Neuroradiol. 2004 Mar;25(3):382-8.
5. Susac J O, Murtagh F R, Egan R A, et al., MRI findings in Susac's syndrome. Neurology. 2003 Dec 23;61(12):1783-7.
6. Sandhya V, Anand N, Susac syndrome. Eye. 2002 Nov;16(6):788-90
7. Sirikci A, Susac syndrome and multiple sclerosis. Arch Otolaryngol Head Neck Surg. 2001 Apr;127(4):468