A 33 year old man with left upper lid swelling
Digital Journal of Ophthalmology 2004
Volume 10, Number 12
December 18, 2004
Volume 10, Number 12
December 18, 2004
There were no visual symptoms of note. He had been diagnosed with Wegener’s Granulomatosis (ANCA positive) 10 years previously, this being treated with immunosuppressive treatment (cyclophosphamide and azathioprine).
He had been off immunosuppressive treatment for 5 years and was well until recent events . Past medical history included hypertension and focal glomerulonephritis secondary to Wegener’s Granulomatosis.
Extra ocular movements revealed limitation of upgaze in the left eye with vertical diplopia. He had 3mm axial proptosis and there was marked conjunctival injection on the lateral aspect of the left eye .
His visual acuities, colour vision, pupillary reflexes, and fundoscopy were normal .

Figure 1
Frontal view demonstrating the left upper lid swelling
Frontal view demonstrating the left upper lid swelling
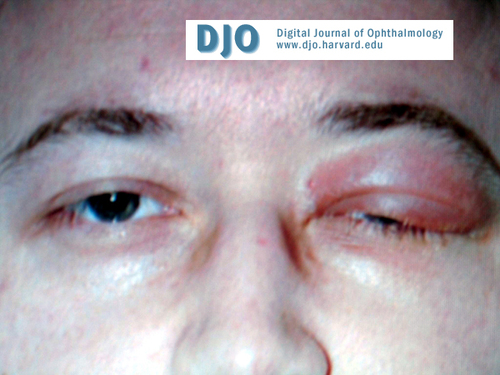
Figure 2
Side view demonstrating collapse of the nasal bridge
Side view demonstrating collapse of the nasal bridge
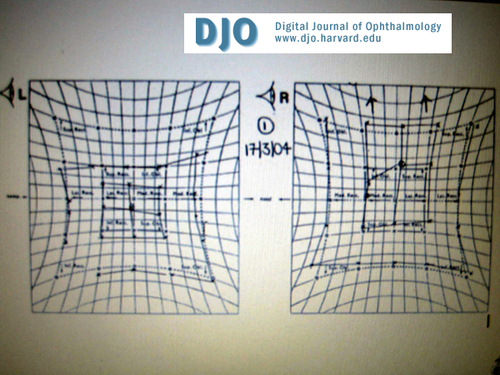
Figure 3
Hess chart showing the restriction in elevation of the left eye
Hess chart showing the restriction in elevation of the left eye
Magnetic Resonance Imaging demonstrated an abnormal ill defined mass filling the left retro orbital space. The abnormal mass extends from the globe to the orbital apex involving some extraocular muscles in particular the lateral rectus.
The abnormal mass appears to extend into the sclera and perhaps through the orbital apex where there may be increased enhancement around the para cavernous area and the anterior temporal lobe on the left .
The optic nerve was surrounded with this abnormal mass but had retained its CSF sheath. There was no paranasal sinus involvement and the right orbit was normal (figure 4 and 5) .
Pathology
Blood tests :
Full Blood Count plus differential , Urea and electrolytes and Autoantibodies were all normal. Anti Neutrophil Cytoplasmic Antibody (ANCA) was positive.
Orthoptic assessment :
The Humphrey threshold 30-2 visual fields were normal .
Hess chart demonstrated hypotropia of the left eye with limitation of upgaze as found on ocular motility (figure 3). The binocular single visual field was present only in the lower part of the visual field.
Histopathology :
Biopsy of the orbital lesion revealed several foci of perivascular inflammation .
The inflammatory cells appear to spill over into the adjacent fat lobules.
There was neutrophilic transmigration through the vessel walls. The closest differential on morphology is that of a panniculitic type of a T cell lymphoma which was ruled out .
The histological features were compatible with a diagnosis of Wegener’s Granulomatosis (figure 6) .
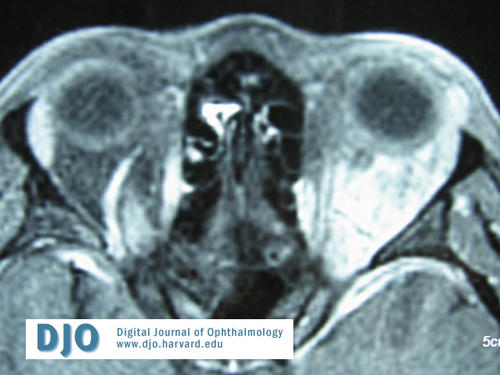
Figure 4
MRI T1 weighted image post contrast demonstrating the abnormal soft tissue mass in the orbit
MRI T1 weighted image post contrast demonstrating the abnormal soft tissue mass in the orbit
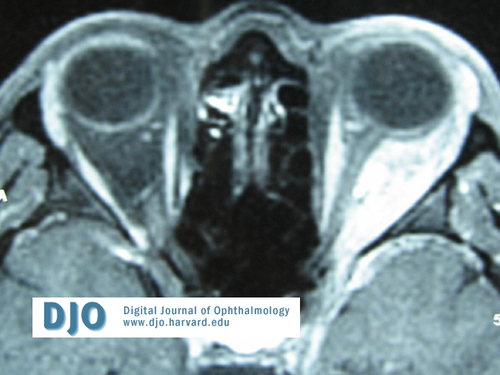
Figure 5
MRI T1 weighted image post constrast . Note the left optic nerve being surrounded by the abnormal mass.
MRI T1 weighted image post constrast . Note the left optic nerve being surrounded by the abnormal mass.
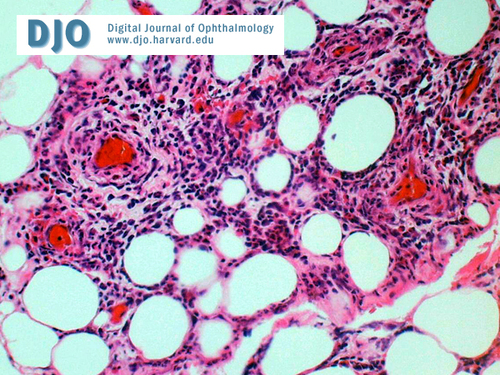
Figure 6
X 20 Magnification. Perivascular inflammation , with spill over of inflammatory cells in the surrounding fat . ( Stain : Hematoxylin-Eosin)
X 20 Magnification. Perivascular inflammation , with spill over of inflammatory cells in the surrounding fat . ( Stain : Hematoxylin-Eosin)
500 mg for 3 days was started with oral cyclophosphamide (160 mg qd) and oral prednisolone (60 mg qd) .
Follow up appointment revealed reduced swelling of the left upper lid. The proptosis of the left eye had resolved and extra ocular movements were full . Repeat MRI demonstrated resolving inflammatory mass in the left orbit.
Lymphoproliferative disorder secondary to previous immunosuppressive treatment
Other malignant disorders
Other inflammatory disorders (e.g Sarcoidosis , Thyroid eye disease , idiopathic)
Orbital infections (e.g Tuberculosis , Syphilis , Bacterial)
WG is classified into three forms. The ‘generalised’ form where systemic vasculitis primarily affects the upper and lower respiratory tracts and kidneys. The ‘limited’ form is confined typically to the respiratory tract and the ‘very limited’ form (which as in our patient) can just affect the orbit. Overall 95% of patients have lung disease, 90% sinus disease and 85% renal disease.[1]
Ocular disease occurs in 50-60% of patients with WG and may be the presenting finding in 13-16%. The most common ocular manifestation is that of orbital involvement (either extending from or independent of sinus involvement).
Presenting symptoms may include awareness of an orbital mass, epiphora, orbital pain and diplopia. Signs may include an orbital mass or proptosis (69%), nasolacrimal duct obstruction (52%), limited ocular rotations (52%), lid erythema and oedema (31%), bony destruction (21%) and reduced visual acuity (17%).[2]
Other frequent findings are conjunctivitis, episcleritis (often preceding scleritis) and peripheral ulcerative keratitis . Less common ophthalmic manifestations include necrotizing scleritis , uveitis , retinitis with venous congestion, optic neuropathy and extra ocular muscle limitation.
Orbital WG may be uni- or bilateral, the latter suggesting disease of greater severity. [3] Our patient had unilateral disease with no sinus involvement which is unusual in relapse of WG.
The main differential diagnosis to consider in this patient was secondary
lymphoproliferative disorder from previous immunosuppressive treatment . However this possibility was unlikely as the histology of the orbital lesion was consistent with a diagnosis of Wegener’s granulomatosis. Although the classic histological triad of vasculitis, tissue necrosis and granulomatous inflammation was not present a review article from the mayo clinic showed that this triad was only present in 54% of orbital WG.[4]
Furthermore the bone marrow trephine and aspirate was normal and a whole body CT failed to demonstrate any evidence of lymphadenopathy .
This is an important distinction to make, as the clinical picture of orbital WG is often similar to that of T-cell lymphomas [5] ( polymorphic reticulosis/lethal midline granuloma) and B-cell lymphomas [6], the treatment of which is radically different.
Nasal and paranasal sinus involvement, resulting in symptoms of progressive nasal obstruction and bloody rhinorrhoea (as opposed to the rapid localized destruction seen in malignant lymphomas) may suggest a diagnosis of WG . The presence of florid lid xanthelasmata has also been reported as being a useful diagnostic pointer in orbital
WG.[7]
A definitive diagnosis of orbital WG requires positive serology and biopsy results suggestive of the disease. Serologic testing for cANCA has been shown to be a useful indicator in cases of ocular inflammation where it is difficult to determine the source of inflammation
( a manifestation of wegener’s granulomatosis).[8]
Computed tomography (CT) and magnetic resonance imaging (MRI) have also proved highly useful. Unenhanced, non fat-supressed T1-weighted MRI sequences provide the best contrast between lesions and normal structures with a marked decrease in the T2 signal being characteristic of WG granulomas.[9 ][3 ]
Changes may be accompanied by signs of dural thickening, enhancements of cerebral infarction and signal abnormalities in the brainstem and white matter. Masses are frequently accompanied by infiltrates of the pterygopalatine fossa and destruction of adjacent bone on CT.
Orbital WG, as with systemic WG, responds well to treatment with
immunosuppressive agents (usually prednisolone and cyclophosphamide). Other regimens have been employed in treatment-resistant cases or when side-effects dictate a different approach . These include the use of such drugs as methotrexate[10], azathioprine and trimethoprim-sulfamethoxazole, the latter having been demonstrated to reduce the rate of relapse.[11] More experimental treatments
have included tumour necrosis factor-blocking drugs, such as Infliximab [12] and Etanercept [13] , and antithymocyte globulin.[14] Surgical intervention has been recommended for refractive cases (where orbital exenteration may be required) and in cases where there is a perceived threat to vision (compression of the optic nerve by a granuloma) .[15]
Successful treatment of orbital WG depends on an early diagnosis. A sound understanding of the various manifestations of the condition is therefore essential.
Untreated, mean survival with WG is 5 months. However approximately 90% of patients respond to cyclophosphamide, with about 75% experiencing complete remission.
orbit: a clinicopathological study of 15 patients. Laryngoscope 2002;112
(11):1945-50
2) Woo TL, Francis IC, Wilcsek GA, et al . Australasian orbital and
adnexal Wegener’s granulomatosis . Ophthalmology 2001;108 (9):
1535-43
3) Provenzale JM, Mukherji S, Allen NB, Castillo M , et al . Orbital
involvement by Wegener’s granulomatosis: imaging findings.
Am J Roentgenol 1996; 166 (4): 929-34
4) Kalina PH, Lie JT, Campbell RJ, Garrity JA. Diagnostic value and
limitations of orbital biopsy in Wegener’s Granulomatosis.
Ophthalomology 1992;99 (1):120-4
5) Berrettini S, Segnini G, Bruschini P, Sellari Franceschini S, et al.
Lethal midline granuloma: a case of Ki-1 lymphoma. Rev Laryngol Otol
Rhinol 1993;114(1):37-42
6) Gawryluk D, Slodkowska J, Dobkowski P, Wiatr E. Diffuse large B-cell
lymphoma mimicking Wegener’s granulomatosis. Pneumonol Alergol Pol
2002;70 (3-4):210-5
7) Tullo AB, Durrington P, Graham E, Holt LP, et al . Florid
xanthelasmata (yellow lids) in orbital Wegener’s granulomatosis.
Br J Ophthalmol 1995;79 (5):453-6
8) Nolle B, Coners H, Duncker G. ANCA in ocular inflammatory
disorders. Adv Exp Med Biol 1993;336:305-7
9) Courcoutsakis NA, Langford CA, Sneller MC , et al. Orbital
involvement in Wegener’s granulomatosis: MR findings in 12 patients.
J Comput Assit Tomogr 1997;21(3):452-8
10) Smith JR, Rosenbaum JT . A role for methotrexate in the
management of non-imfectious orbital inflammatory disease .
Br J Ophthalmol 2001;85(10):1220-4
11) Stegeman CA, Tervaert JW, Kallenberg CG . Co-trimoxazole and
Wegener’s granulomatosis: more than a coincidence. Nephrol Dial
Transplant 1997 ;12(4):652-5
12) Kleinert J, Lorenz M, Kostler W, et al. Refactory Wegener’s
granulomatosis responds to tumour necrosis factor blockade. Wien Klin
Wochenschr 2004;116(9-10): 334-8
13) Stone JH, Uhlfelder ML, Hellmann DB, Crook S , et al . Etanercept
combined with conventional treatment in Wegener’s granulomatosis : a
six-month open-label trial to evaluate safety . Arthritis Rheum. 2001;44
(5):1149-54
14) Kool J, de Keizer RJ, Siegert CE. Antithymocyte globulin treatment
of orbital Wegener granulomatosis: a follow-up study . Am J Ophthalmol
1999;127(6):738-9
15) Duncker G, Gross WL, Nolle B , et al.Orbital involvement in
Wegener’s granulomatosis. Klin Monatsbl Augenheilkd. 1992;201(5):309-
16