A 16 year old with Blurred Vision
Digital Journal of Ophthalmology 2003
Volume 9, Number 4
December 29, 2003
Volume 9, Number 4
December 29, 2003
- A 16 year old girl presented with gradually decreasing vision OS for a duration of 12 months.
Past ocular history:
- Iris coloboma OD
- Retinochoroidal colobomas OD & OS
Medical & Family history:
- nil
Medications:
- nil
OD 20/60 OS 20/60
Anterior segments:
OD: Inferonasal iris coloboma (Figure 1)
OS: Normal
Fundus examination:
OD: Extensive inferior chorioretinal coloboma (Figure 2)
OS: Partial inferior chorioretinal coloboma (Figure 3), optic disc pit (Figure 3), and extensive serous elevation of the macula (Figure 4)
Applanation tonometry: Normal (OU)
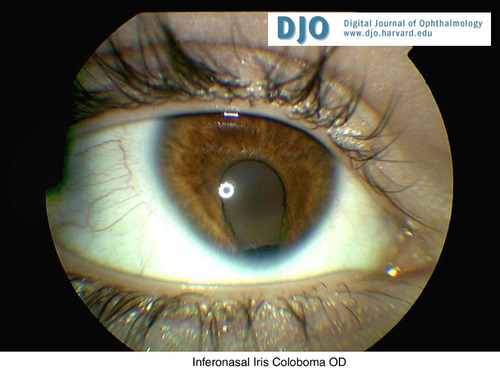
Figure 1
Inferonasal Iris Coloboma OD
Inferonasal Iris Coloboma OD
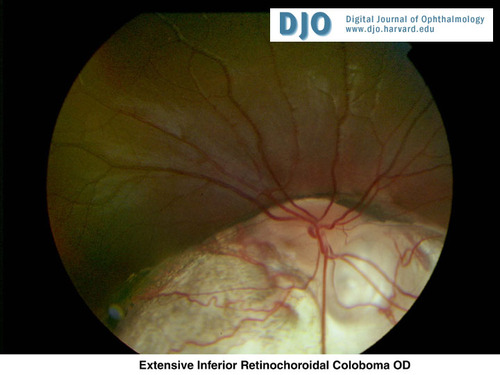
Figure 2
Extensive Inferior Retinochoroidal Coloboma OD
Extensive Inferior Retinochoroidal Coloboma OD
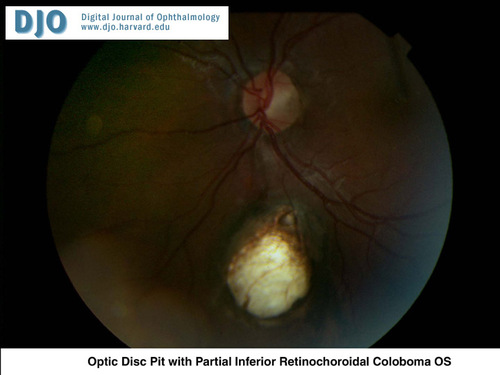
Figure 3
Optic Disc Pit with Partial Inferior Retinochoroidal Coloboma OS
Optic Disc Pit with Partial Inferior Retinochoroidal Coloboma OS
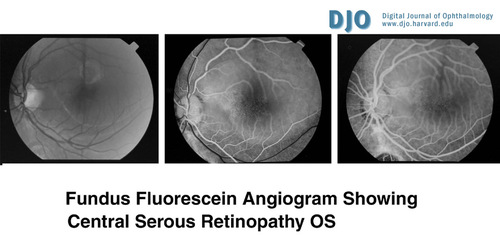
Figure 4
Fundus Fluorescein Angiogram demonstrating central serous retinopathy
Fundus Fluorescein Angiogram demonstrating central serous retinopathy
and laser photocoagulation to the left eye. She was followed up for a
period of 12 months. There has been no improvement in the visual
acuity but the retina remains flat in the operated eye.
2. Macular or paramacular hole
3. Peripheral retinal detachment with pooling of subretinal fluid in the macula
4. Peripheral chorioretinal lesions leading to exudative detachment extending into the macular area.
In 30-40% of the cases of congenital optic disc pits, there is a serous elevation of the macula resulting in reduced visual acuity (5,6). The pathogenesis of this is unclear. The subretinal fluid could be derived from the vitreous or the cerebrospinal fluid in the subarachnoid space around the optic disc. Other macular lesions that can be seen include macular edema, macular hole, macular cyst and pigmentary mottling.
Spontaneous reattachment of the retina has been reported but is rare(1). Macular detachment is associated with a very poor visual prognosis. Any treatment that allows the sensory retina to reattach is desirable in comparison to allowing the detachment to follow its natural course. The various treatment modalities include ocular patching and mannitol, bed rest, steroids, photocoagulation, diathermy, cryotherapy, drainage of subretinal fluid, scleral buckling procedures and intraocular gas injection. The above treatments have variable results and the best treatment has not been determined. The following treatment plan has been recommended (7): If there is no permanent macular damage, observation is advised for 3 months. If spontaneous reattachment occurs, the patient can proceed for laser treatment. If there is no reattachment bed rest and semi pressure eye patching for 2 days followed by laser and observation for 2 months is suggested. Further failure to reattach can be treated with intraocular gas and laser. If failure to reattach persists, vitrectomy with air/fluid exchange and additional laser is recommended.
1. Sugar HS. Congenital pits in the optic disc and their equivalents associated with
submacular fluid. Am J Ophthalmol 1967; 298-307
2. Singerman LJ, Mittra RA. Hereditary optic disc pit and iris coloboma in three
generations of a single family. Retina 2001; 273-275
3. Gass M, Donald J. Serous detachment of the macula secondary to congenital pit of
the optic nerve head. Am J Ophthalmol 1969; 821-41
4. Dureau P, Attie-Bitach T, Salomon R, Bettembourg O, Amiel J, Uteza Y et al.
Renal coloboma syndrome. Ophthalmology 2001; 1912-1916.
5. Theodossisdias G. Evolution of congenital pit of optic disc with macular detachment
in photocoagulated and nonphotocoagulated eyes. Am J Ophthalmol 1977; 620-31
6. Hayreh SS. Fluids in the anterior part of the optic nerve in health and disease. Surv
of Ophthalmol 1978; 1-25
7. Schatz H, Mc Donald HR. Treatment of sensory retinal detachment associated with
optic nerve pit or coloboma. Ophthalmology 1988; 178-86