A 5 year old girl who failed her school vision screening
Digital Journal of Ophthalmology 2004
Volume 10, Number 5
February 19, 2004
Volume 10, Number 5
February 19, 2004
The slit lamp exam was remarkable for several distinctive findings in each eye. The right eye had a crescent-shaped, equatorial, fibrovascular plaque on the anterior lens capsule with a finger extending to the center of the optical axis of the capsule, causing distortion and capsular striae. There was central dragging of the ciliary processes and medial subluxation of the lens (Figure 1). Numerous remnants of the tunica vasculosa lentis (TVL) were present, and an anterior TVL vessel extended from the iris to the anterior surface of the plaque. The iris vasculature appeared engorged and contained many radial corkscrew vessels (Figure 2). There were vessels in the angle and also areas of angle closure. The left eye showed a broad area of iris pigment epithelial adhesion to the anterior lens capsule with persistent pupillary hairpin vessels present temporally (Figure 3). An elongated hairpin annular iris vessel was also seen extending across the superior pupil. Similar engorged corkscrew iris vessels were present. Perfused remnants of the posterior vasa hyaloidea propria and posterior TVL vasculature were seen in both eyes.
The posterior segment was evaluated by indirect ophthalmoscopy with fundus photography and fluorescein angiography using the RetCam (Massie Labs, Pleasanton, CA). The posterior segment findings were similar in both eyes. The maculas and peripheral retinas were normal in appearance, with well-developed foveas. There was a perfused hyaloid artery originating at the optic nerve head, which coursed anteriorly to the retrolental space. Fluorescein angiography demonstrated slow but complete perfusion of both hyaloid arterial trees (Figure 4). The hyaloid vessel then ramified into temporal coursing vasa hyaloidea vessels (1 in the right eye, 3 in the left eye), which anastomosed with the iris vasculature as described above. There was significant fluorescein leakage at the site of the anastomoses between these vessels in the left eye (Figure 4B). Anterograde flow was seen throughout the systems in both eyes except for an anastomosis in the left eye that showed retrograde perfusion from the iris back to a branch of the posterior tunica vasculosa lentis. Individual red blood cells could be seen flowing through the vessels of the posterior TVL on the angiogram study, consistent with a low-flow arterial system. Doppler ultrasound identified the hyaloid artery and measured the flow velocity within the artery in the mid-vitreous at 0.01-0.02 M/sec (Figure 5).
The vitreous was markedly abnormal in both eyes. In the right eye, the vitreous cavity appeared to be "optically empty" in the nasal hemisphere. There was an oval cystic structure in the vitreous cavity that was adherent to the hyaloid artery in the mid-vitreous (Figure 6). The cyst appeared to be anchored at the vitreous base temporally and was 1.0 x 1.6 cm in size by ultrasound (Figure 7). The left vitreous cavity also appeared to be "optically empty". Several translucent cystic masses were seen in the temporal periphery in the region of the vitreous base. One appeared to be a small oval mass of formed vitreous. Ultrasound studies showed these masses to be oval or spherical cysts within the vitreous cavity, each of which appeared to be anchored at the level of the vitreous base (Figure 8A). A hemispheric cyst fixed to the region of the vitreous base was also seen (Figure 8B). T2-weighted MRI images detected the large cyst in the left eye (Figure 9).
Figure 1
Figure 1. Plaque on the anterior lens capsule in the right eye (arrow). Medial subluxation of the lens and an irregular shape to the margin to the capsule are evident (arrowheads). Medial dragging of the ciliary body processes is also seen (asterisks).
Figure 1. Plaque on the anterior lens capsule in the right eye (arrow). Medial subluxation of the lens and an irregular shape to the margin to the capsule are evident (arrowheads). Medial dragging of the ciliary body processes is also seen (asterisks).
Figure 2
Iris vessels and vessels of the tunica vasculosa lentis (TVL) in the right eye. Several small remnants of the TVL are seen along the papillary margin. A single larger vessel anastomoses with vessels of the posterior TVL and vasa hyaloidea propria (arrow). Large radial corkscrew vessels are seen throughout the iris.
Iris vessels and vessels of the tunica vasculosa lentis (TVL) in the right eye. Several small remnants of the TVL are seen along the papillary margin. A single larger vessel anastomoses with vessels of the posterior TVL and vasa hyaloidea propria (arrow). Large radial corkscrew vessels are seen throughout the iris.
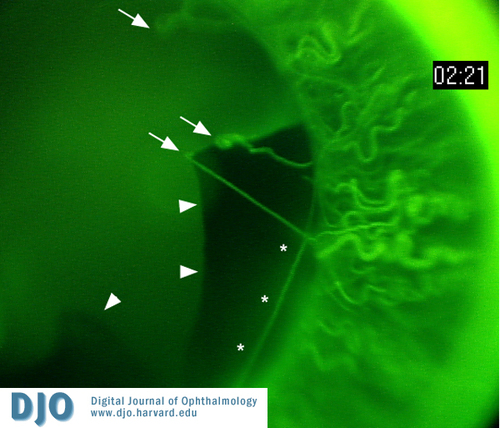
Figure 3
Iris vessels and vessels of the tunica vasculosa lentis (TVL) in the left eye. A broad area of iris pigment epithelial adhesion to the anterior lens capsule is present (arrowheads). Elongated TVL vessels are dragged medially (arrows) and an annular iris vessel is also seen medial to the pupillary margin (asterisks). Large radial corkscrew vessels are seen throughout the iris.
Iris vessels and vessels of the tunica vasculosa lentis (TVL) in the left eye. A broad area of iris pigment epithelial adhesion to the anterior lens capsule is present (arrowheads). Elongated TVL vessels are dragged medially (arrows) and an annular iris vessel is also seen medial to the pupillary margin (asterisks). Large radial corkscrew vessels are seen throughout the iris.
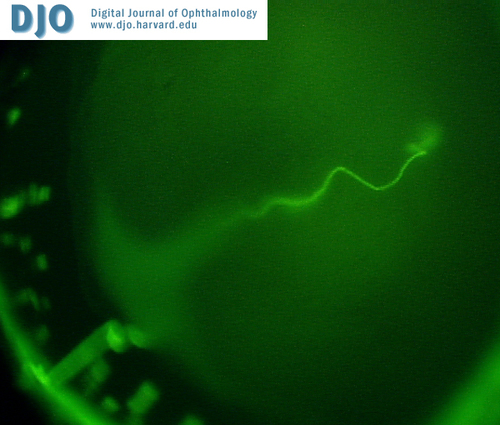
Figure 4a
Fluorescein angiogram of the right hyaloid arterial tree.
Fluorescein angiogram of the right hyaloid arterial tree.
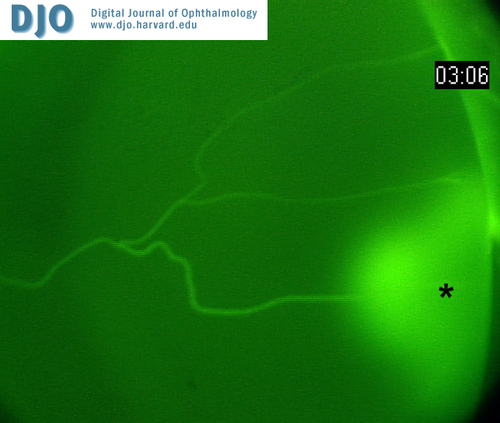
Figure 4b
Fluorescein angiogram of the left hyaloid arterial tree. Dye leakage is seen at the inferior-most anastomosis of the posterior TVL (asterisk).
Fluorescein angiogram of the left hyaloid arterial tree. Dye leakage is seen at the inferior-most anastomosis of the posterior TVL (asterisk).
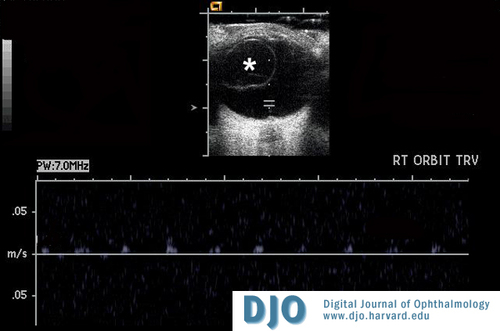
Figure 5
Dynamic ultrasound of the right eye. A large vitreous cyst is present in transverse section (asterisk). Flow analysis of the hyaloid artery in the posterior vitrous cavity demonstrates pulsatile arterial flow at 0.01-0.02 M/sec.
Dynamic ultrasound of the right eye. A large vitreous cyst is present in transverse section (asterisk). Flow analysis of the hyaloid artery in the posterior vitrous cavity demonstrates pulsatile arterial flow at 0.01-0.02 M/sec.
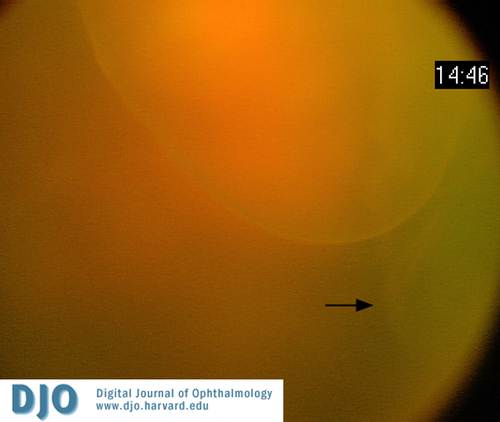
Figure 6
RetCam image of the large vitreous cyst in the right eye. A smaller cyst appears to be present adjacent to it (arrow).
RetCam image of the large vitreous cyst in the right eye. A smaller cyst appears to be present adjacent to it (arrow).
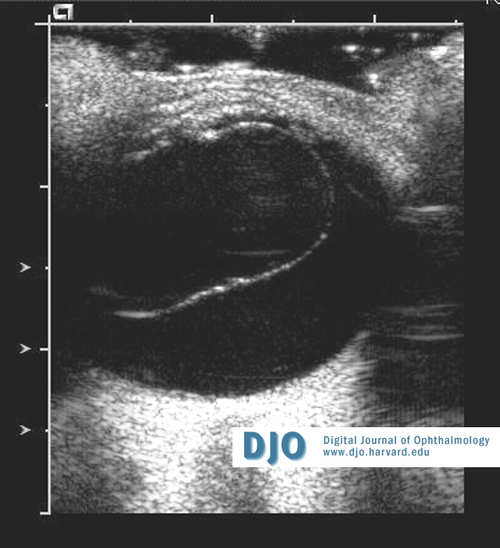
Figure 7
Ultrasound image of the right eye showing a large vitreous cyst in sagital section.
Ultrasound image of the right eye showing a large vitreous cyst in sagital section.
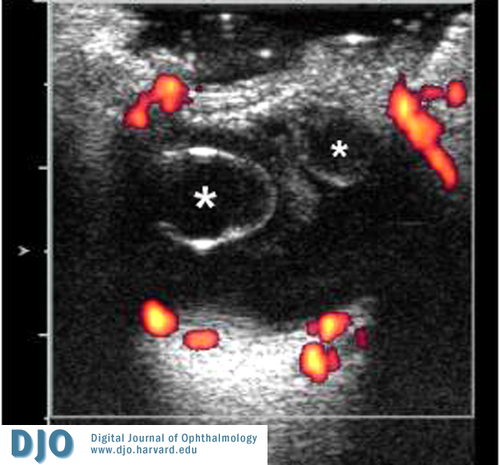
Figure 8a
Ultrasound studies showing multiple, small vitreous cysts in transverse section.
Ultrasound studies showing multiple, small vitreous cysts in transverse section.
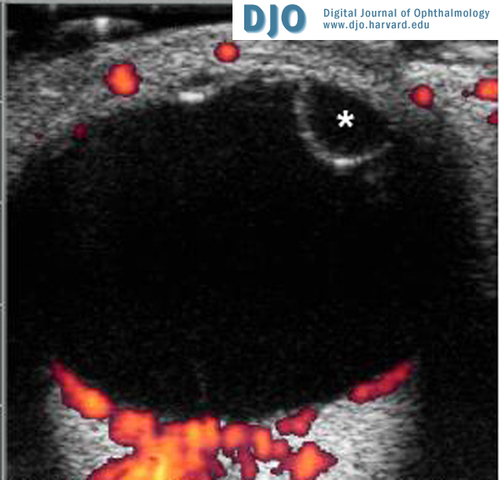
Figure 8b
Ultrasound studiy showing hemispheric cyst at the vitreos base in the left eye.
Ultrasound studiy showing hemispheric cyst at the vitreos base in the left eye.
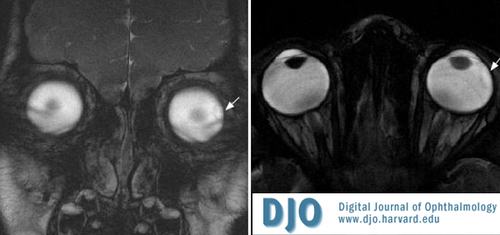
Figure 9
T2-weighted MRI images showing the large vitreous cyst in the left eye (arrows).
T2-weighted MRI images showing the large vitreous cyst in the left eye (arrows).
Congenital vitreous cysts, although rare, are well-known ocular developmental anomalies, and several case series reviews have been published. (3,4) Vitreous cysts have been reported as free-floating masses or with anterior or posterior attachments. (5,6) Rare reports have described cysts in association with prepapillary hyaloid remnants. (7) We present an unusual case of a child with bilateral PFV associated with multiple bilateral congenital vitreous cysts.
Discussion
Congenital cysts of the vitreous are rare ocular developmental anomalies. Numerous isolated cases have been reported and occasional associations with other congenital ocular anomalies have been noted as described above. Vitreous cysts have been reported in cases of ocular inflammatory disease and following surgical trauma (8,9); however, the origin and embryology of congenital vitreous cysts remains controversial. Previous authors have speculated that vitreous cysts originate from various sites including the ciliary processes, the pars plana ciliaris, colobomata, Bergmeister's papilla, and cystic transformation of the hyaloid artery or its glial sheath. (2,7,10) Vitreous cysts have also been reported in association with juvenile retinoschisis (11) and retinitis pigmentosa. (12)
The embryological development of the vitreous is a 3-step process. The primary vitreous begins to develop at about 3 weeks of age and is complete by about 9 weeks. The hyaloid artery and its ramifications, the vasa hyaloidea propria and tunica vasculosa lentis, develop from mesodermally derived cells during formation of the primary vitreous. Following this, the inner retina begins liberating collagen, and Mueller cells and hyalocytes secrete the hyaluronic acid of the secondary vitreous. Formation of the secondary vitreous displaces the primary vitreous centrally, the condensed junction of which forms Cloquet's canal. The tertiary vitreous is secreted last and condenses to form the suspensory ligaments of the lens (zonules). Formation of the secondary vitreous is completed by the end of the first trimester, whereupon the vascular components of the hyaloid system begin a slow process of involution regulated in part by macrophage-mediated apoptosis. Recent studies of knockout mice have suggested possible roles for TGF-B2, TBDN-1, p53, and Arf in mediating vascular regression during vitreous development. (13,14)
Three vitreous cysts examined by light and/or electron microscopy have been reported in the literature. One developed following multiple retinal detachment surgeries and was found to contain gliotic retinal tissue, likely due to seeding of the vitreous with retinal tissue. (9) The origin of a congenital cyst was posited to be from the pigment epithelium of the pars plicata ciliaris in another patient. (10) A third report of a congenital vitreous cyst showed it to be composed of heavily pigmented cells connected by tight junctions and containing microvilli and melanosomes at various stages of maturity. Immunohistochemical analysis was positive for carbonic anhydrase. From these findings and location of the cyst in Cloquet's canal, the authors concluded that the cyst was a congenital choristoma of the primary hyaloidal system. (15)
These authors and others have recognized the association of congenital vitreous cysts with common embryologic remnants of hyaloid and vitreous development. (7,8,16) Cysts have been associated with anterior hyaloid remnants (Mittendorf dots) and posterior remnants (Bergmeister papillae), sometimes with connections between the structures. Our patient had different types of cysts in her eyes and at different locations. There was one large cyst in the right eye that appeared to be tethered to the hyaloid artery in the mid-vitreous. There were several smaller cysts in the left eye that appeared to be anchored at the level of the vitreous base. There were no attachments between the hyaloid artery and these structures in the left eye; however, small attachments to residual vessels of the vasa hyaloidea propria or posterior vessels of the TVL may have been present and not identified.
It has been previously proposed, and this case suggests, that vitreous cyst formation may result from events that lead to aberrant regression of the hyaloid vasculature during ocular embryogenesis and may reflect cystic transformation of the glial remnants of the hyaloid vasculature. (2,6-8,17) The mechanism of cyst formation in the anterior vitreous is thought to be due to similar cystic transformation of more anterior hyaloid vessels that ramify throughout the secondary vitreous. Myxomatous and osseous changes in the associated anterior fibrous tissue have also been reported. (2) This patient represents an unusual and extreme example of multiple congenital, bilateral vitreous cysts in association with PFV.
These studies supported in part by an unrestricted Departmental grant from Research to Prevent Blindness Inc., New York, NY, and The Plough Foundation, Memphis, TN.
1. Goldberg MF. Persistent fetal vasculature (PFV): An integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV) LIV Edward Jackson Memorial Lecture. Am J Ophthalmol 124:587-626 (1997)
2. Duke-Elder S. System of Ophthalmology. Vol 3. Anomalies of the Vascular System. St. Louis: CV Mosby; 1963:764-782.
3. Tansley JO. Cyst of the vitreous. Trans Am Ophthalmol Soc 8:507-509 (1899)
4. Feman SS, Straatsma BR. Cyst of the posterior vitreous. Arch Ophthalmol 91:328-329 (1974)
5. Saracco JB, Roumagnou J, Naudin B. Kyste cong¨¦nital du corps vitr¨¦. Bull Soc Ophtalmol Fr 71:55-58 (1971)
6. Philippot M, Philippot J, Philippot V. Kyste congenital du corps vitre. Bull Soc Ophtalmol Fr 84:1243-1246 (1984)
7. Francois J. Pre-papillary cyst developed from remnants of the hyaloid artery. Br J Ophthalmol 34:365-368 (1950)
8. Bullock JD. Developmental vitreous cysts. Arch Ophthalmol 91:83-84 (1974)
9. Asiyo-Vogel MN, El-Sayed E-H, Laqua H. Ultrastructural features of a solitary vitreous cyst. Retina 16:250-254 (1996)
10. Orellana J, O¡¯Malley RE, McPherson AR, Font RL. Pigmented free-floating vitreous cysts in two young adults. Ophthalmology 92:297-302 (1985)
11. Lusky M, Weinberger D, Kremer I. Vitreous cyst combined with bilateral juvenile retinoschisis. J Ped Ophthalmol Strab 25:75-76 (1988)
12. Roveda JM, Iribarren R, Sampaolesi R. Pigmentary retinopathy and vitreous cyst. Arch Oftalmol Buenos Aires 28:208-214 (1953)
13. Paradis II, Liu C-Y, Salka S, et al. Tubedown-1 in remodeling of the developing vitreal vasculature in vivo and regulation of capillary outgrowth in vitro. Dev Biol 249:140-155 (2002)
14. McKeller RN, Fowler JL, Cunningham JJ, et al. The Arf tumor suppressor gene promotes hyaloid vascular regression during mouse eye development. Proc Nat Acad Sci 99:3848-3853 (2002)
15. Nork TM, Millecchia LL. Treatment and histopathology of a congenital vitreous cyst. Ophthalmology 105:825-830 (1998)
16. Steinmetz RL, Straatsma BR, Rubin ML. Posterior vitreous cyst. Am J Ophthalmol 109:295-297 (1990)
17. Lisch W, Rochels R. [Pathogenesis of congenital vitreous cysts (German)]. Klin Monatsbl Augenheilkd 195:375-378 (1989)
