A 13 year-old girl with right eye swelling
Digital Journal of Ophthalmology 2004
Volume 10, Number 7
May 14, 2004
Volume 10, Number 7
May 14, 2004
Near vision OD N8 OS N6
Exophthalmometry OD 18mm OS 13mm
The right eye had a hypotropia and exotropia in primary position. Motility examination was notable for limitation of elevation, adduction, diplopia in all positions of gaze.
Anterior Segment examination was notable OD for dilatation of conjunctival vessels, obscuration of upper eyelid crease, and sluggish pupillary reaction. An afferent pupillary defect was not present.
Fundus examination OD demonstrated dilated, tortuous veins and retinochoroidal folds in the posterior pole.
Examination of the left eye was unremarkable.

Figure 1.
Appearance at presentation.
Appearance at presentation.
Hb 12.5 gm%, ESR 58, WBC 9200 (N78 L20 E2 M0). Creatinine, Platelet Count, Blood sugar, Bleeding and clotting time were all normal. Serology for HIV and Hepatitis B was negative.
CT Scan demonstrated pansinusitis and an abscess in the right superior orbit (Figure 2).
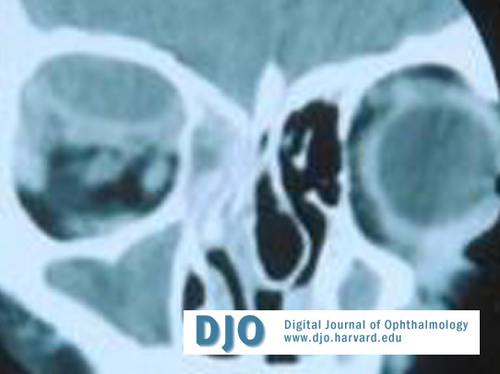
Figure 2.
CT scan demonstrating a sub-periosteal abscess in the right orbit.
CT scan demonstrating a sub-periosteal abscess in the right orbit.
Some improvement in proptosis, edema were noticed but not adequate.
The right orbital abscess was drained by passing a 22 gauge Venflon cannula into the orbit below the supraorbital foramen. Pus was noted in the cannula. The needle was removed and negative pressure was applied to the cannula which was still in place. 6 to 7 cc thick greenish pus was aspirated into the syringe. Pressure was applied on eyelids maintained for 5min. Proptosis considerably reduced. A tight bandage was applied on eye and patient was extubated. Systemic antibiotics and NSAID’s were continued for 5 days post operatively.
The gram stain and cultures were negative.
On the first post-operative day, exophthalmometry demonstrated 2 mm proptosis OD. Visual acuity was OD 6/9 OS 6/6. Extraocular movements improved markedly, but diplopia presisted on elevation. Pupil examination was normal. Fundus exam revealed marked reduction in choroidal folds.
At 15 days post op., the examination had returned to normal (Figure 3). The patient was asked to observe OD closely and report immediately if fever or proptosis recurred as the abscess wall was still in place. No surgical treatment was performed for the pansinusitis, however follow up was advised.
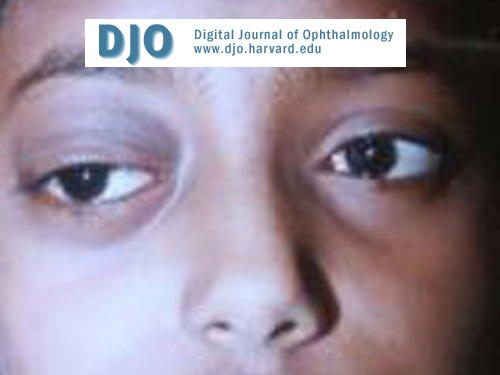
Figure 3.
Post-operative appearance.
Post-operative appearance.
The mean age at presentation is 20-31 years [5 ,10]. They commonly present as an acute febrile illness, with proptosis, lid swelling, chemosis, impaired ocular motility, visual defects, pupillary abnormalities,colour vision deficits, and field defects [2,9] .Orbital infections are classified as [7]:
Group I Preseptal cellulitis, inflammatory edema, congestion
Group II Orbital infiltration& Mass effects & Functional deficits
Group III Subperiosteal abscess
Group IV Orbital abscesses & Mass effects
Group V Intracranial extension of inflammation into cavernous sinus.
Differential diagnosis of orbital cellulitis includes leukaemia [11], rhabdomyosarcoma [2], metastatic tumors [2], retinoblastoma [12], hemangiomata [13], lymphangiomata [14], dermoid cysts [15], neurofibromas with associated with bony defects and meningoencepahloceles [16], hydatid cysts of the orbit [17], and orbital varices [18].
Complications include intracranial spread leading to meningitis, intracranial abscess, cavernous sinus thrombosis, blindness [19,20,21], and death.
Etiological agents implicated include Staphylococcus aureus, Streptococcus pneumoniae, Hemophilus influenzae, anaerobes, Propionibacterium acnes, Pseudomonas, Pneumocystis, mixed infections and rarely parasites, fungi & mollicutes [1, 10,22,23,24,25] . Leukocytosis and blood cultures are unreliable. CT scans with coronal sections are useful [26]. It is important to note that computerized scans cannot predict whether the mass represents a haematoma, an exudate or a transudate [20]. MRI is frequently necessary for patients with intracranial infections [27, 28]. Ultrasonography is a useful adjunct [28]. Fine needle aspiration biopsy has been used to diagnose orbital metastatses [29].
Aggressive parenteral antibiotics with judicious surgical intervention constitute the mainstay of treatment [30]. Empirical treatment of proptosis with systemic steriods should be avoided as infections will be aggravated [24]. Cephalosporins every 12hrs for 7-10 days, followed by oral cephalosporins for 7 days are most commonly used drugs. B-lactamase resitant penicillins are also useful. Chloramphenicol, clindamycin, vancomycin are alternatives if initial treatment is not successful due to resistance. It is important not to overlook the possibility of the abscess being tuberculous. Anti-inflammtory medications, such as NSAIDs, may help reduce inflammation.
Criteria for nonsurgical treatment of subperiosteal abscess include: age < 9 yrs, normal visual acuity, normal visual fields, normal motility, no cranial nerve palsy, and no afferent pupillary defect [30,31].
Indications for surgical treatment include worsening of clinical parameters, such as decreasing visual acuity [5]. Abscess drainage becomes necessary in 50% to 70% of cases [5]. Standard technique of drainage involves making a skin incision closest to the abscess site, deepening it to the periosteum, and then inserting an instrument into the subperiosteal space of the orbit to break the abscess wall. Aspiration of the contents to avoid intra-orbital spread is essential.
In this context, CT guided orbital abscess drainage can be performed via CT guidance, as is performed for biopsies of optic nerve tumors [21,32]. It is important to note the maximum length of the needle for drainage of orbital abscesses is 3.75 cm [21]. A Venflon 22 gauge cannula is 3.5 cm long and is incapable of reaching the intracranial space through the superior orbital fissure. The Venflon cannula (22 gauge) is inserted in one of the oblique quadrants rather than directly above or below the globe to avoid accidental perforation. The cannula is closely watched to see if blood / pus are noted as the Venflon is introduced. Once pus is seen the inner needle is removed and a syringe with negative pressure is attached to the Venflon facilitating quick drainage into the syringe. The material obtained is subjected to microbiological examination (Gram stain, Ziehl Neilsen & Fungal Stains, aerobic and anaeorbic culture), and cytopathological examination [21,31] .
In spite of CT Scan guidance, adequate anesthesia, and guarded insertion of the Venflon cannula, complications can occur. The most common complication reported is hematoma formation which resolves spontaneously. Loss of extra ocular movements, ptosis, blindness, death are other complications [21,32].
Failure to drain may suggest a mass lesion, orbital pseudotumor or tumor, and indicate the need for an open biopsy, or may suggest that the cannula is not within the abscess and requires re-positioning. Microbiological and cytopathological examination of aspirates from the orbit is essential and may provide a clue to the diagnosis
The procedure of draining orbital/subperiosteal abscesses using a Venflon cannula may be tried on a large scale. We recommend a larger trial by the ophthalmic fraternity.
1. Antonio A.V.Cruz, MD, Marisa M. Mussi Pinhata, MD, Patrician M S Akaishi, MD, Luciana Cattebeke, MD, Jose Torranda Silva, MD, Jorge Elia Jr, MD,
Neonatal Orbital Abscess
Ophthalmology 108 : 2316-2320, 2001
2. Levine Robert A, Putterman Allan M,
Orbital and Adnexal Tumors
Principles and Practice of Ophthalmology Ed Gholam Peyman, Donald R Sanders, Morton F Goldberg, W.B. Saunders Company Vol III page 2169
3 Gamble R.
Acute inflammations of the orbit in children
Arch Ophthal 10 : 483-497, 1933
4 Jarrett WH II, Gutman FA
Ocular complications of infection in the paranasal Sinuses.
Arch Ophthal 81: 683 , 1969
5 Weiss A, Friendly D, Eglin K, Chang M, Gold B.
Bacterial, periorbital, orbital cellulitis in childhood
Ophthalmology Vol. 90 : 195-203, 1983.
6. Haynes RE, Gramblett HG
Acute Ethmoiditis, its relationship to orbital cellulitis .
Am J Disease Child 114 : 261, 1967.
7. Chandler James R, Langen Brunner David J, Stevens Edward R.
The pathogenesis of Orbital complications in Acute sinusitis
Laryngoscope 80 : 1414 - 1428, 1970
8. Fovilla - Canales JL, Nava V, Tovillay Pomar JL
Orbital and periorbital infections.
Curr. Opin Ophthalmol 12(5) : 335 - 341, 2001
9. Durboraw Catherine E, Stasior George D, Krohel Gregory B..
Orbital cellulitis and Abscesses, Section 376.01 Current Ocular Therapy, V Edition Ed Fredrick T. Fraunfelder, F. Hampton Roy, John Randall
W.B.Saunders Company 2000
10. Heier Jeffery S., Gardner Thomas A, Hawes Michael J., Mc Guere Keith A, Wallton William T, Stock Jonathan
Proptosis as the initial presentation of Fungal sinusitis in Immunocompetent patients
Ophthalmology 102 : 713-717, 1995
11. Kincaid MG, Green WR
Ocular and orbital involvement in Leukaemia
Surv. Ophthal 27 : 211-232, 1983
12. Carbagal UM
Metastases in Retinoblastoma
Am J O phth 48:47 , 1959
13. Hood. C
Cavernous Haemangioma of the Orbit
Arch Ophthal 83:49 - 1970
14. Reese AB, Howard GM
Unusual manifestations of ocular lymphangioma and lymphangiectasis.
Surv Opthal 18:226 – 1973
15. Pfeiffer RL, Nicholl RJ
Dermoid and Epidermoid tumors of the orbit
Arch. Ophthal 40:639-1948
16. Burrows EH
Bone changes in orbital neuro fibromatosis
Br. J.Radiology 36:549 – 1963
17. Baghdassarian SA, Zakharia H
Hydatid cyst: Report of 3 cases
Am J Ophthal 71:1081 – 1971
18. Lloyd OAS, Wright JE, Morgan G
Venous malformations in orbit
Br. J. Ophthal 55:505 – 1971
19 Hartstein ME, Stein Vurzel, MD, Cohen CP
Intracranial abscess as a complication of subperiosteal abscess of orbit
Ophthal Plast Reconstr Surg 17(6) : 398-403, Nov 2001
20. Hodges E., Tabbara K.F.
Orbital cellulitis - Review of 23 cases from Saudi Arabia
Br. J Ophthal Vol 73 : 205-208, 1989
21. Kennerdell J.S., Dubois PJ, Dekker A, Johnson BI
CT guided fine needle aspiration biopsy of orbital optic N Tumors
Ophthalmology Vol 87:491-496, 1980
22. Donahue SP, Schwartz GS
Preseptal cellulitis and orbital cellulitis in childhood – A changing microbiological spectrum
Ophthal Vol 105: 1902-1905,1998
23. Heier Jeffery S., Gardner Thomas A, Hawes Michael J., Mc Guere Keith A, William T Wallton, Jonathan Stock
Proptosis as the initial presentation of Fungal sinusitis in Immunocompetent patients
Ophthalmology 102 : 713-717, 1995
24. Sullivan T J, Aylward GW, Wright GE
Actinomycosis of orbit
Br. J. Ophthal Vol 76: 505-506,1992.
25. Kronish JW, Johnson TE, Gilberg SM, Corrett GF, McLeish WM, Scott KR
Orbital infections in patients with HIV infections.
Ophthalmology Vol 103: 1483-1492,1996
26. Wirostko E, Johnson L, Wirostko B
Chronic Orbital Inflammatory disease,parasitation of
orbital leucocytes by mollicute like organisms
Br. J. Ophthal Vol 73: 865-870, 1989
27. Younnis RT, Anand VK, Davidson B
The role of computed tomography and magnetic resonace imaging in patients with sinusitis with complications.
Lanyngoscope 112 (2) 224 - 249 Feb 2002.
28. Char H Devran, Miller Theodore, Kroll Stewart
Orbital Metastases: Diagnosis and Course
Br. J. Ophthal Vol 81: 386-390, 1997
29 Krohel G, Krauns H, Winnick V.
Orbital abscess
Ophthalmology (Rochester) 89, 492-501, 1982
30. Bergin DJ, Wright JE
Orbital cellulitis
Br J Ophthal Vol 70 : 174-178 1986
31. Gracia H George, Harris J Gerald
Criteria for nonsurgical treatment of subperiosteal abscess of the orbit
Analysis of outcomes 1988-1998
Ophthalmology Vol 107: 1454-1456,2000.
32. Liu D
Complications of fine needle aspiration biopsy of orbit
Ophthalmology Vol 92 : 1768-1771, 1985.
