46-year-old gentleman with bilateral blurry vision and photophobia for 6 months.
Digital Journal of Ophthalmology 2004
Volume 10, Number 4
February 3, 2004
Volume 10, Number 4
February 3, 2004
Past Medical History: Hypertension
Past Ocular History: Presbyopia
Current Medications: Denies
Allergies: Denies
Occupation: House Father
Habits: Smokes 5-6 cigars per day and consumes 6 alcoholic beverages per day.
Pupillary examination - round reactive, no afferent defect detected.
Ocular Motility - Full ductions and saccades.
Color Vision - able to read the control plate only in both eyes.
Tensions - 17 mm Hg OD, 21 mm Hg OS
Fundus Examination - please see photos
OD Fundus Photo
Presenting Fundus Photo OD
Presenting Fundus Photo OD

OS Fundus Photo
Presenting OS Fundus Photo
Presenting OS Fundus Photo
Ancillary Testing:
Goldmann Visual Field Testing - Bilateral ceco-central scotomas
Normal Hearing
Hemoglobin - 13.5 g/dl (low)
Hematocrit - 39.4 % (low)
White cells - 10.1 (normal)
RPR - non-reactive
Vitamin B12 - 466 pg/ml (normal)
Folic Acid 7.4 ng/ml (normal)
PCR analysis for mitochondrial DNA mutations found in Lebers Hereditary Optic Neuropathy - Negative for any mutation
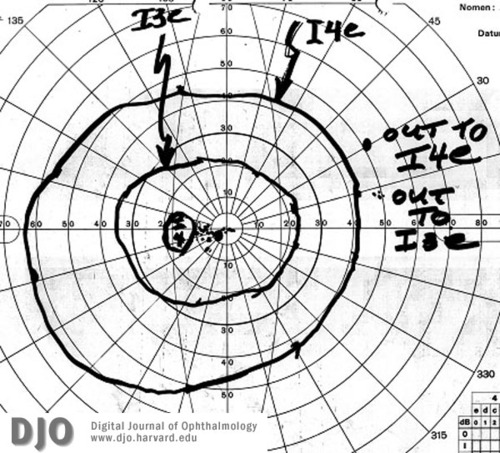
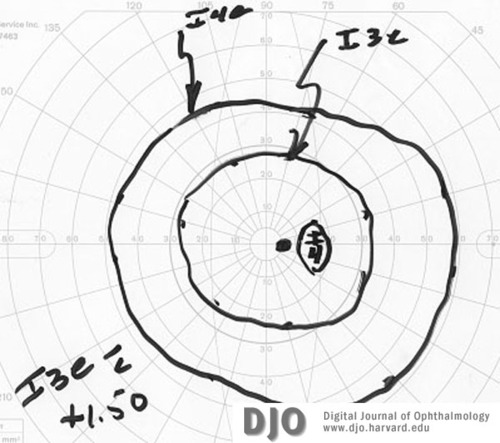
OS Visual Field
Presenting OS Visual Field
Presenting OS Visual Field
OD Visual Field
Presenting OD Visual Field
Presenting OD Visual Field
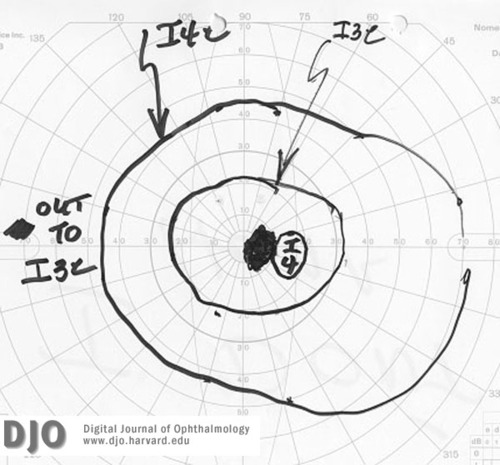
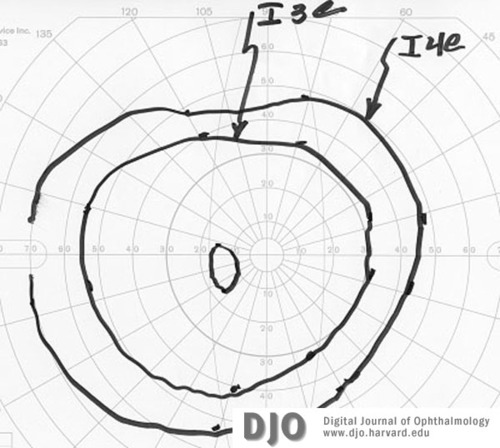
OS Visual Field
OS Visual field 2 months into treatment
OS Visual field 2 months into treatment
OD Visual Field
OD Visual Field 2 months into treatment
OD Visual Field 2 months into treatment
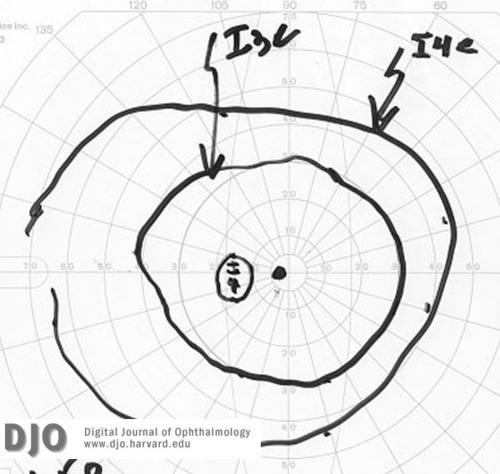
OS Visual Field
OS Visual Field 6 months into treatment
OS Visual Field 6 months into treatment
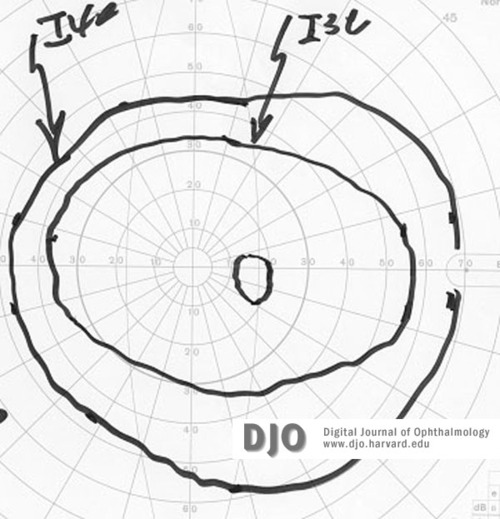
OD Visual Field
OD Visual Field 6 months into treatment
OD Visual Field 6 months into treatment
2. Retinopathies may cause metamorphopsia, night blindness, photisms, and delayed glare recovery
3. Neural causes
Dominantly inherited (Kjer's)
Mitochondrially inherited (Leber's)
Inflammatory/Demyleinating optic neuropathies
Infiltration or compression
Pernicious anemia
A multifactoral etiology is postulated since only a minority of patients who smoke develop this disease and no dose dependent correlation has been discovered. Cyanide toxicity from cigarette smoke and relative malabsorption of Vitamin B12 from the gut have been postulated as mechanisms, but not proven (1). Alcohol has also been postulated to be a co-factor in this disease process, however, alcohol alone has not been proven to be toxic to the visual pathways. Low serum vitamin B12 levels have been suspected as one factor (2).
Patient with Tobacco Amblyopia can have any level of visual acuity. It presents as a painless, progressive bilateral optic neuropathy with visual loss, dyschromatopsia, and ceco-central scotomas on visual field testing. Nystagmus, ptosis, and ophthalmoplegia can be present if the patient is experiencing Wernicke's encephalopathy. The optic nerve appears pale and the rest of the fundus usually appears normal. An evanescent peripapillary retinopathy characterized by hemorrhages and dilated, tortuous vessels in the nerve fiber layer has been described in a case series (3).
Treatment consists of hydroxocobalomin injections or oral replacement therapy and cessation of smoking. Nonetheless, patients such as the one presented here who have continued to smoke and who receive vitamin B12 do improve. Previous studies have shown that hydroxocobalomin is superior to cobalomin alone in the treatment of these patients. Administration of the medications with an internist and close follow up with visual field testing is recommended when following these patients.
2. Foulds WS, Chisholm IA, Bronte-Stewart JM, et al: Vitamin B12 absorption in tobacco amblyopia. Br J Ophthalmol 53:393, 1969.
3. Frisén L: Fundus changes in acute nutritional amblyopia. Arch Ophthalmol 101:577, 1983.