A 40 year old woman with decreased vision for one year
Digital Journal of Ophthalmology 2003
Volume 9, Number 2
June 23, 2003
Volume 9, Number 2
June 23, 2003
Past medical history: Hypertension
Past surgical history: Repair of 2 left-sided intracranial aneurysms 18 months prior (a 3mm saccular aneurysm arising from the left middle cerebral artery and 2mm supraclinoid left internal carotid artery aneurysm)
Family History: Sister with an intracranial aneurysm that required
surgery
Meds: Nadolol
OS: 16/70, pinhole to 16/15
Near vision: OU: J1+ without correction
Manifest refraction: OD: -0.75-0.50 x 170= 16/15
OS: -0.75-0.25 x 15 = 16/15
Pupils: + Afferent defect OS
Color vision: OD 10/10
OS 8/10
Amsler Grid: full OU
Motility: full OU
Exophthalmometry: 14mm OU
Intraocular pressure: 12mm Hg OU
Anterior segment: Anterior segment exam revealed no abnormalities
Posterior Segment: There are numerous angioid streaks which appear as tortuous, dark brown cracks at the level of Bruch's membrane and radiate peripherally from the optic nerve. The midperipheral fundus has a peau d'orange appearance. The left fundus demonstrates angioid streaks as well as optic nerve pallor
Skin: There was a waxy, papular, plucked chicken texture to the patient's skin.

Anterior Segment Exam
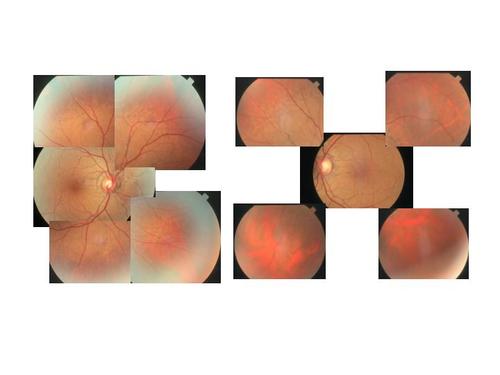
Posteior Segment Exam

Skin Examination
Fluorescein angiogram: The early flurorescein angiogram of the left eye shows linear window defects and areas of staining corresponding to the angioid streaks. The late flurorescein findings of the left eye show some persistent areas of staining, but no leakage or pooling.
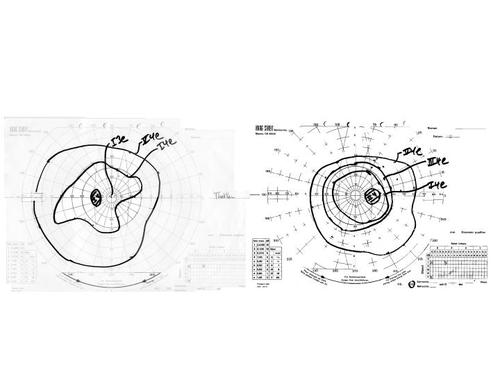
Visual Fields
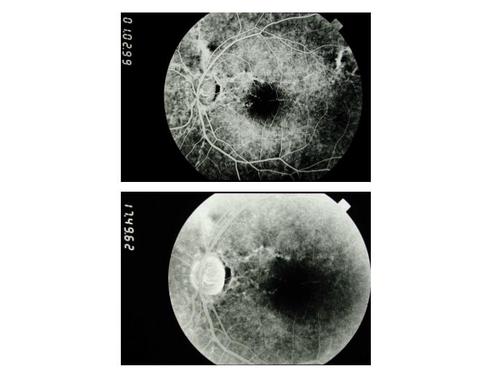
Fluorescein Angiogram
1. Idiopathic (45%)
2. Pseudoxanthoma Elasticum (34%)
3. Paget's Disease of Bone (10%)
4. Sickle cell disease/trait or other hemoglobinopathies (6%)
5. Ehlers-Danlos syndrome (rare)
6. Myopia
Pseudoxanthoma elasticum (PXE) is a disorder of elastic connective tissue that affects multiple organ systems: namely, the eyes, skin, GI tract and cardiovascular system. It is rare, with an incidence of 1 per 160,000 and is more commonly found in females. The inheritance, most commonly autosomal recessive, can also be sporadic or dominant with variable penetrance.
The pathophysiology of PXE involves progressive calcification of elastin fibers throughout the body, resulting in elastic tissues in various vessels and organs becoming more brittle. Studies have shown that PXE patients have an abnormal gene on Chromosome 16 that codes for a transmembrane transporter protein (1). One theory is that this defect results in abnormal calcium accumulation in the extracellular elastic matrix. Another theory is that this transporter causes production of abnormal glycosaminoglycans in the extracellular matrix, which somehow promotes excessive calcium deposition. The true biomolecular pathophysiology is still largely unknown.
On ophthalmic exam, approximately 85% of patients with PXE have angioid streaks in the retina. Conversely, approximately one third of patients with angioid streaks have pseudoxanthoma elasticum. Other systemic diseases that should be considered in a patient with angioid streaks include Paget's disease of bone, sickle cell disease/trait, other hemoglobinopathies, and Ehlers-Danlos syndrome.
Angioid streaks appear as breaks or dehiscences in Bruch's membrane with overlying pigment epithelial atrophy and disruption of the underlying choriocapillaris. These are usually bilateral and found posterior to the equator. It is thought that the extrinsic forces of the extraocular muscles on a calcified, brittle Bruch's membrane are a possible cause of these breaks, which are acquired and progressively worsen with age. Early hyperfluorescence of the streaks on fluorescein angiogram is secondary to the overlying pigment epithelial atrophy. Persistent staining of the streaks late in the fluorescein angiogram is another characteristic finding.
Frequent ophthalmic examinations are mandated in patients with angioid streaks because of their tendency to develop choroidal neovascular membranes (CNVM). CNVM in patients with PXE frequently are vision threatening, and a majority of these individuals become legally blind by age 50. Features of angioid streaks that predict a poor prognosis are length, distance from the fovea, and whether they are diffuse, or appear like a cracked egg shell(2). Because even minor ocular trauma can cause subretinal hemorrhages, patients should be encouraged to use eye protection and avoid contact sports. Laser photocoagulation has been used to treat CNVM in these patients, with limited success(3). There is a case reported of a successful treatment of CNVM in a patient with PXE with submacular translocation(4).
Other ophthalmic findings in PXE include a peau d'orange fundus appearance, which due to RPE degeneration presumably secondary to alterations in Bruch's membrane. Salmon spots can also be seen and appear as small, round yellow lesions also due to RPE atrophy and degeneration of Bruch's membrane. Patients with PXE have also been reported to have a higher incidence of macular and optic nerve drusen.
Patients with PXE tend to have systemic disorders related to calcification of elastin in blood vessels and skin. Skin findings in these patients include a plucked chicken appearance consisting of waxy, yellow papules commonly seen on the neck, axillae, and periumbilical regions. Elastin calcification in blood vessels leads to hypertension, intracranial aneurysms, cerebral ischemia, coronary artery disease, and gastrointestinal bleeds. Intracranial aneurysms in these patients are potentially life threatening and should always be considered in patients with PXE and neurological symptoms. Ischemic optic neuropathy can occur in these patients as a result of gastrointestinal bleeds(5) or status-post intracranial aneurysm surgery from ischemia or direct surgical manipulation(6).
2. Mansour AM et al. Macular Degeneration in Angioid Streaks. Ophthalmologica 1988;197:36-41.
3. Singerman LJ, Hatem G. Laser Treatment of Choroidal Neovascular Membranes in Patients With Angioid Streaks. Am J Ophthal 1993;116:414-423.
4. Roth DB et al. Macular Translocation for Subfoveal Choroidal Neovascularization in Angioid Streaks. Am J Ophthal 2001;131 (3):390-392.
5. Yap EY et al. Visual Loss Associated With Pseudoxanthoma Elasticum. Retina 1992;12(4):315-319.
6. Rizzo JF. Visual Loss After Neurosurgical Repair of Paraclinoid Aneurysms. Ophthalmology 1995;102(6):905-10.