A 57-year-old woman with periocular pain
Digital Journal of Ophthalmology 2021
Volume 27, Number 3
September 3, 2021
Volume 27, Number 3
September 3, 2021
Download PDF
Further history revealed that 6 years earlier, the patient was referred by optometry to an outside glaucoma specialist for concerns of angle closure in the setting of narrow angles. She reported symptoms of periocular headache and photophobia. At that time, records indicated that she had narrow, occludable angles in both eyes with closed presentation on gonioscopy and normal IOPs of 16 mm Hg in each eye. Prophylactic LPI was recommended and performed at that time.

Figure 1.
The initial visual field (A, B) and optical coherence tomography (OCT) of the retinal nerve fiber layer (RNFL). The average retinal nerve fiber layer thickness was 85 ?m for the right eye (C) and 77 ?m for the left eye (D). The average cup-to-disc of the optic nerve head for both eyes is 0.62. The axial length and the anterior chamber depth for both eyes was 23.20 mm and 2.82 mm, respectively.
The initial visual field (A, B) and optical coherence tomography (OCT) of the retinal nerve fiber layer (RNFL). The average retinal nerve fiber layer thickness was 85 ?m for the right eye (C) and 77 ?m for the left eye (D). The average cup-to-disc of the optic nerve head for both eyes is 0.62. The axial length and the anterior chamber depth for both eyes was 23.20 mm and 2.82 mm, respectively.
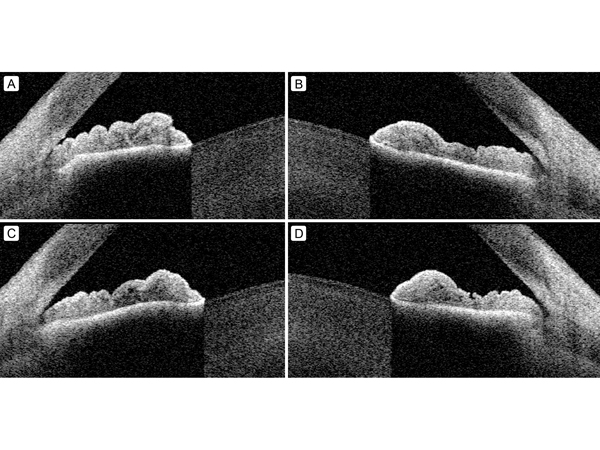
Figure 2.
Initial anterior segment OCT imaging of the right eye (A) and left eye (B) showing lens vaulting, narrow angles and some mild plateau iris configuration. Anterior segment OCT imaging of the right eye (C) and left eye (D) 3 days after laser iridoplasty showing mild improvement in plateau iris configuration.
Initial anterior segment OCT imaging of the right eye (A) and left eye (B) showing lens vaulting, narrow angles and some mild plateau iris configuration. Anterior segment OCT imaging of the right eye (C) and left eye (D) 3 days after laser iridoplasty showing mild improvement in plateau iris configuration.
One month later, the patient returned to the outpatient urgent care clinic for worsening headache. Her IOP was within normal limits in each eye, and examination revealed no change suggestive of acute angle closure or other acute ophthalmic disease. She was referred to the Emergency Department for further work-up of her severe headache symptoms. She continued to present emergently for severe headache over the next several months. Computed tomography (CT) of the head with and without contrast revealed no intracranial abnormalities. In addition, CT angiography was normal. Labs, including complete blood count, comprehensive metabolic panel, urine analysis, and urine pregnancy tests were all unremarkable. In the Emergency Department, the patient’s symptoms eventually resolved with intravenous fluids and pain medication, including ketorolac.
The patient then returned for delayed ophthalmology follow-up in the glaucoma clinic 7 months after ALPI, when she demonstrated stable IOP in each eye and unchanged examination. The continued headache symptoms were thought to be less likely related to primary angle closure syndrome given the quality of the symptoms and stability of her examination; however, atypical presentation of angle closure was not ruled out. The patient was scheduled for close follow-up at 2 months, with repeat OCT RNFL imaging.
In the course of her continued multidisciplinary workup for her headache symptoms, the patient was referred to otorhinolaryngology, where she received a CT scan of the face and neck, which demonstrated calcification of the stylohyoid ligament (Figure 3). Otorhinolaryngology diagnosed the patient with Eagle syndrome and attributed the recurrent periorbital pain and headaches to this phenomenon. They recommended the patient for stylohyoidectomy.
The patient then returned to scheduled 2-month glaucoma follow-up, at which point her OCT testing demonstrated progression of inferior and superior RNFL thinning in the left eye in spite of stable IOPs (Figure 4). Her diagnosis was changed from primary angle closure syndrome to primary angle closure glaucoma. Therapeutic options were discussed with the patient, including medical management with topical eyedrops versus surgical management with cataract extraction. In spite of the provider’s preference for a trial of medical therapy, the patient opted to proceed with cataract extraction. As evidenced by the EAGLE Study, which demonstrated the efficacy and cost-effectiveness of clear-lens exchange as primary treatment for primary angle closure glaucoma, cataract extraction with insertion of intraocular lens was performed along with goniosynechiolysis in the left eye, followed after three weeks by the right eye.(1)
Shortly following these surgeries, the patient underwent trans-oral styloidectomy. On postoperative week 4 after right eye surgery, IOP was 18 mm Hg in each eye, and the patient reported slight lessening of periocular pain. The patient continues to follow-up every 6 months in the glaucoma clinic, with stable IOPs and visual fields off of pressure-lowering eye drops. Overall, after styloidectomy the patient’s neck and ear pain has resolved, although she continues to report occasional headaches and currently sees Neurology for management.
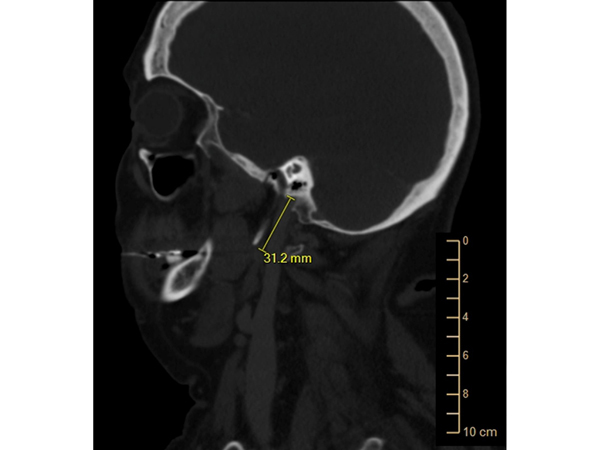
Figure 3.
Computed tomography (sagittal cut) of the head and neck demonstrating elongation of the styloid process characteristic in stylohyoid or Eagle syndrome.
Computed tomography (sagittal cut) of the head and neck demonstrating elongation of the styloid process characteristic in stylohyoid or Eagle syndrome.
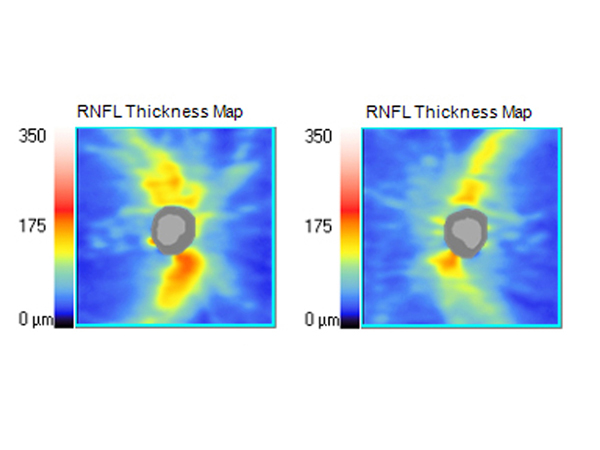
Figure 4.
OCT of the RNFL 10 months after initial presentation demonstrating progressive thinning of the nerve fiber layer in the left eye. The average retinal nerve fiber layer thickness was 83 ?m for the right eye (A) and 73 ?m for the left eye (B).
OCT of the RNFL 10 months after initial presentation demonstrating progressive thinning of the nerve fiber layer in the left eye. The average retinal nerve fiber layer thickness was 83 ?m for the right eye (A) and 73 ?m for the left eye (B).
Eagle syndrome, also known as stylohyoid syndrome, was first described by Eagle in 1937 and has since been associated with multiple complications, including carotid compression (presyncope and syncope) and cervicofacial pain.(2-3) The syndrome is characterized by calcification of the stylohyoid ligament or elongation of the styloid process, either by congenital abnormality or acquired (ie, following trauma). The incidence of stylohyoid abnormalities has been reported to be 22%-84%; however, the incidence of associated pain is only 4%-10%. In such cases, anatomic abnormalities are often present bilaterally, yet pain typically presents unilaterally.(4) Eagle syndrome typically presents with vague cervicofacial pain complaints and, as in our case, has been described as mimicking other diseases.(5,6)
Intermittent periocular headache is a common and nonspecific clinical symptom. However, in the setting of other ophthalmic findings, such as anatomically narrow angles, gonioscopic synechiae, elevated IOP, or glaucomatous optic neuropathy, this symptom is suggestive of intermittent angle closure. In patients who present with normal IOP during their routine office visits, persistent pain suggestive of angle closure presents a clinical challenge that requires prophylactic treatment or continued workup of alternative etiologies. The ultimate diagnosis of Eagle syndrome in our patient helped to clarify the pathology the patient’s pain and also freed the clinical team from anchoring on angle closure as the primary etiology of the patient’s symptoms. Additionally, our patient did ultimately present with glaucomatous optic neuropathy, and the history of this angle pathology confounded the work-up of her nonspecific pain symptoms, which were at least in part secondary to nonophthalmic disease. To our knowledge, this case is the first report of Eagle syndrome masquerading as intermittent angle closure.
Literature Search
PubMed was searched on June 22, 2020, for English-language results, using the following terms: Eagle syndrome and glaucoma.
2. Eagle W. Elongated styloid processes: report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol 1949;49:490-503.
3. Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg 2017;159:34-8.
4. Correll RW, Jensen JL, Taylor JB, et al. Mineralization of the stylohyoid–stylomandibular ligament complex: a radiographic incidence study. Oral Surg Oral Med Oral Pathol 1979;48:286-91.
5. Cohn JE, Othman S, Sajadi-Ernazarova K. Eagle syndrome masquerading as a chicken bone. Int J Emerg Med 2020;13:1.
6. Cohn JE, Scharf J. Eagle syndrome. J Am Osteopath Assoc 2018;118:629.