A 47-year-old man with a necrotic wound after trauma
Digital Journal of Ophthalmology 2021
Volume 27, Number 2
May 17, 2021
Volume 27, Number 2
May 17, 2021
Download PDF
Intraocular pressure (IOP) was 66 mm Hg in the right eye and 22 mm Hg in the left eye. The right upper and lower eyelids were significantly more swollen than the left, and the bulbar conjunctiva of the right eye demonstrated more chemosis than the left; however, the corneas remained clear in both eyes. Use of a Desmarres retractor was necessary to open the right eye, which may have exerted mechanical pressure on the globe and contributed to the elevation in the measured IOP. Despite repeated instillation of brimonidine, timolol, and dorzolamide eye drops in the right eye, his IOP remained dangerously elevated. Acetazolamide could not be used because of the patient’s acidosis while intubated. A lateral canthotomy and cantholysis was subsequently performed, with significant improvement in the IOP, eyelid edema, and chemosis over the next several days. His external examination returned to baseline and his IOP normalized in the right eye over the following 2 weeks with continuation of his hypotensive eye drops.
The patient was followed daily in the hospital by our ophthalmology service and remained stable until an acute overnight change, when the patient developed a large, necrotic, ulcerating lesion near the site of the initial laceration (Figure 2).

Figure 1.
External photograph on presentation to the surgical intensive care unit, 6 days prior to initial ophthalmic examination.
External photograph on presentation to the surgical intensive care unit, 6 days prior to initial ophthalmic examination.

Figure 2.
External photograph after eschar formation, 2 weeks after initial examination and 24 hours after right eye external examination returned to baseline.
External photograph after eschar formation, 2 weeks after initial examination and 24 hours after right eye external examination returned to baseline.
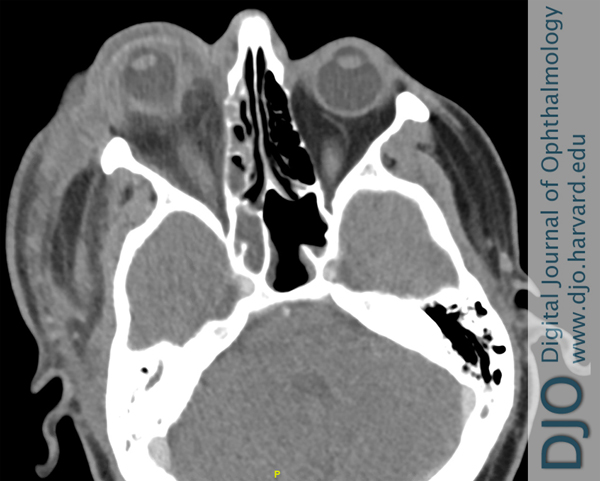
Figure 3.
Axial computed tomography (CT), with contrast, of the head and orbits obtained 11 days after consultation as a result of eschar formation, showing marked proptosis of the right eye, with edema and inflammation extending beyond the septum but no drainable fluid collection. There is also presence of ethmoid sinus disease.
Axial computed tomography (CT), with contrast, of the head and orbits obtained 11 days after consultation as a result of eschar formation, showing marked proptosis of the right eye, with edema and inflammation extending beyond the septum but no drainable fluid collection. There is also presence of ethmoid sinus disease.
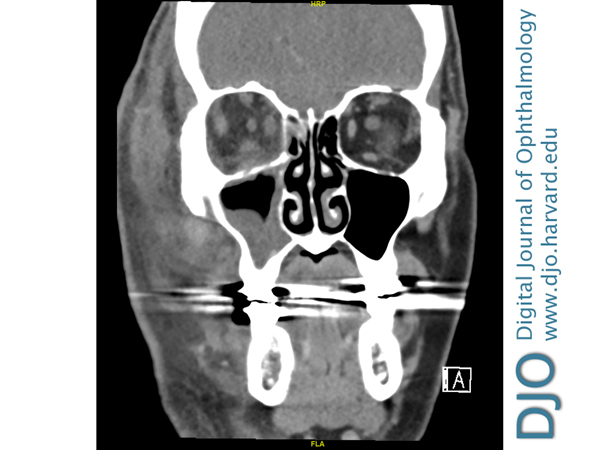
Figure 4.
Coronal CT of the head and orbits, with contrast, showing edema of the right post septal orbit and maxillary sinus disease.
Coronal CT of the head and orbits, with contrast, showing edema of the right post septal orbit and maxillary sinus disease.
Surgical pathology consistently revealed angioinvasive mucormycosis in all specimens. There were also areas of intraneural invasion (Figure 5). This result was confirmed on staining with periodic acid-Schiff and Grocott-Gomori methenamine silver. No organisms were ever grown in culture.
He was started on liposomal amphotericin B, isavuconazole, and micafungin. The dressing placed over the wound was also soaked in amphotericin B and replaced several times throughout the day. After adequate surgical debridement, the patient’s exenteration site was clear of any visible eschar and began to granulate, showing optimistic signs of healing. Repeat CT imaging did not demonstrate any concern for evidence of further active fungal infection. On discharge, the patient completed 6 weeks of amphotericin B. He continued isavuconazole for a total of 8 months and had no recurrences of mucormycosis after discharge. The patient eventually received a skin graft and was fitted with a silicone prosthesis with an excellent aesthetic outcome.
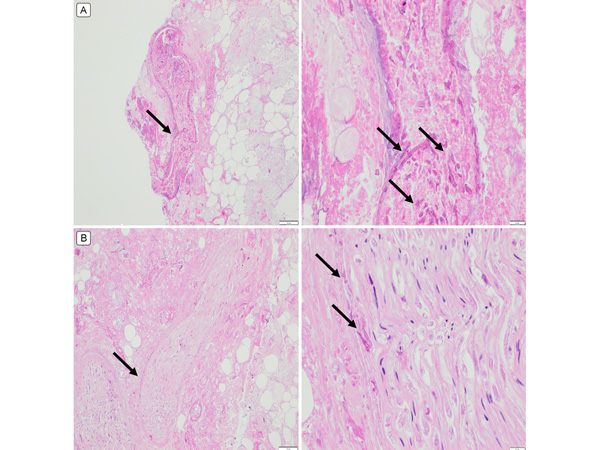
Figure 5.
A, Periodic acid Schiff (PAS) stain demonstrating angioinvasion of mucormycosis (arrows). The right panel demonstrates higher magnification of the area demarcated by the arrow in the left panel. B, PAS stain of the optic nerve showing focal areas of necrosis with invasive mucormycosis (black). Right panels, original magnification ×40; left panels, ×400.
A, Periodic acid Schiff (PAS) stain demonstrating angioinvasion of mucormycosis (arrows). The right panel demonstrates higher magnification of the area demarcated by the arrow in the left panel. B, PAS stain of the optic nerve showing focal areas of necrosis with invasive mucormycosis (black). Right panels, original magnification ×40; left panels, ×400.
Necrotizing fasciitis is a relatively uncommon infection that can present following skin trauma. It can occur in any part of the body, but most cases involve the extremities. Initial signs and symptoms include swelling, fever, pain, and erythema. Diagnosis may be difficult in the early phase of the disease because it mimics other superficial skin infections, such as cellulitis or abscess.
Orbital cellulitis is another infection that may occur as a consequence of trauma. Signs and symptoms include eyelid erythema and swelling, pain with eye movement, ophthalmoplegia, decreased visual acuity, proptosis, and chemosis. The diagnosis is clinical; however, imaging can reveal the degree of orbital involvement.
Invasive fungal disease, in this case specifically mucormycosis, exhibits many of the same signs and symptoms listed above. Mucor is a ubiquitous fungus often found in soil and should be considered in any case of trauma associated with soil that results in an acute eschar resembling necrotizing fasciitis.
Signs of mucormycosis can appear similar to the presentation of necrotizing fasciitis as well as preseptal or orbital cellulitis. This mimicry can complicate the diagnosis and highlights the importance of surgical pathology on initial debridement. On examination, periorbital edema, proptosis, chemosis, visual acuity deficits, and ophthalmoplegia may be noted. In the initial phases of mucormycosis, infected tissue appears erythematous, eventually progressing to a violaceous color and ultimately becoming a black, necrotic eschar.(5) It is associated with a high mortality rate, even with treatment. It has been estimated that even with the combination of surgical debridement and amphotericin B, the mortality rate for mucormycosis exceeds 50%.(5)
Our patient displayed signs of a rapidly progressive, necrotizing infection as evidenced by his physical examination and imaging findings. Based on the extensive facial involvement and acute progression of his disease, we suspected etiologies with a fulminant time course. However, necrotizing fasciitis and orbital cellulitis appeared to be plausible explanations. It was difficult to make a single unifying diagnosis until pathology results returned. His only predisposing risk factors were trauma from the motor vehicle accident contaminated by soil and iron overload, which was most likely secondary to the >30 blood transfusions he received during the treatment of his motor vehicle injury.
Treatment success is dependent on early recognition of symptoms as well as early initiation of medical and surgical therapies. However, identification of early disease may prove difficult, as infected tissue may appear normal.(5) The keystone of treatment is the combination of liposomal amphotericin B and surgical debridement.(1) Additionally, there is anecdotal evidence that adjunctive intraorbital irrigation with amphotericin B may improve treatment outcomes.(6) Proof-of-concept experiments have suggested that iron chelation with deferiprone may be effective in the treatment of mucormycosis in a DKA mouse model.(7) However, the drug was associated with a narrow therapeutic window, and doses above 100 mg/kg proved to be toxic. Of note, deferoxamine, another iron chelator, has been suggested to be a siderophore for several species of fungi and is associated with increased incidence of mucormycosis.(7)
In conclusion, this 47-year-old man with no history of diabetes mellitus or immunocompromised state—both commonly understood risk factors for mucormycosis— developed a rapidly progressive, necrotic facial lesion due to mucormycosis. He received more than 30 blood transfusions, which likely led to an iron-overloaded state. Secondary hemochromatosis appears to be associated with the development of mucormycosis. It would be an inadequately supported claim to assert that iron overload was a direct causative factor for mucor infection or proliferation in this patient; nevertheless, it is plausible that iron overload played an important role in its emergence, given the patient’s many transfusions. This case illustrates the importance of recognizing iron overload as a possible risk factor to consider in mucormycosis and suggests that the differential diagnosis in patients that present with scenarios similar ours be broadened accordingly.
2. Singla K, Samra T, Bhatia N. Primary cutaneous mucormycosis in a trauma patient with Morel-Lavallée lesion. Indian J Crit Care Med 2018;22:375-7.
3. McNab AA, McKelvie P. Iron overload is a risk factor for zygomycosis. Arch Ophthalmol 1997;115:919-21.
4. Artis WM, Fountain JA, Delcher HK, Jones HE. A mechanism of susceptibility to mucormycosis in diabetic ketoacidosis: transferrin and iron availability. Diabetes 1982;31:1109-14.
5. Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev 2005;18:556-69.
6. Joos ZP, Patel BC. Intraorbital irrigation of amphotericin B in the treatment of rhino-orbital mucormycosis. Ophthalmic Plast Reconstr Surg 2017;33:e13-16.
7. Ibrahim AS, Spellberg B, Edwards J Jr. Iron acquisition: a novel perspective on mucormycosis pathogenesis and treatment. Curr Opin Infect Dis 2008;21:620-5.