A 29-year-old man with bilateral megalocornea
Digital Journal of Ophthalmology 2021
Volume 27, Number 2
April 18, 2021
Volume 27, Number 2
April 18, 2021
Download PDF
Anterior chamber examination was unremarkable, with no fibrillary material, iris atrophy, Krukenberg spindles, inflammatory/pigment cells, or midperipheral iris transillumination defects. Anisocoria was not present and the right eye pupil was atropinized after surgery. There was prominent iridodonesis and phacodonesis in both eyes (Video 1). Both lenses were clear and centered. Initial untreated intraocular pressure (IOP) was 56 mm Hg in the right eye and 18 mm Hg in the left eye. Four-mirror indentation gonioscopy showed 360° of open angles to ciliary body bands in both eyes, with more pigmented posterior trabecular meshwork (PTM) in the right eye (+4) compared with the left eye (+2). See Figure 2. There was no exophthalmos. Optic disc examination revealed advanced optic nerve cupping in the right eye and a normal disc in the left eye (Figure 3).
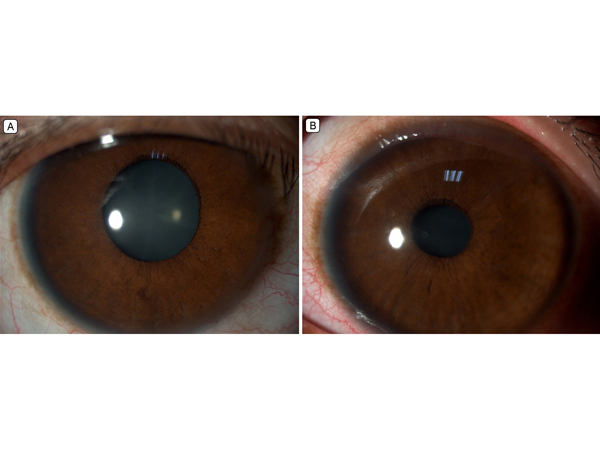
Figure 1.
Anterior segment photographs. A, Right eye, after placement of glaucoma drainage device, showing an enlarged cornea, with a horizontal diameter of 14 mm (the pupil was dilated postoperatively). B, Left eye at presentation showing an enlarged cornea with a 14 mm horizontal diameter.
Anterior segment photographs. A, Right eye, after placement of glaucoma drainage device, showing an enlarged cornea, with a horizontal diameter of 14 mm (the pupil was dilated postoperatively). B, Left eye at presentation showing an enlarged cornea with a 14 mm horizontal diameter.
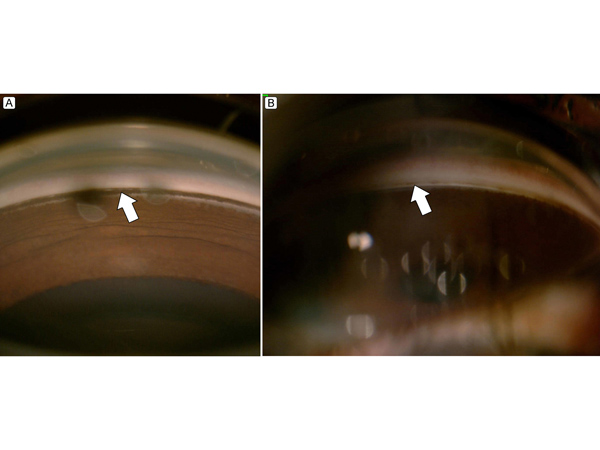
Figure 2.
A, Gonioscopy of the right eye showing +4 posterior trabecular meshwork pigmentation (arrow). B, Gonioscopy of the left eye showing +2 posterior trabecular meshwork pigmentation (arrow).
A, Gonioscopy of the right eye showing +4 posterior trabecular meshwork pigmentation (arrow). B, Gonioscopy of the left eye showing +2 posterior trabecular meshwork pigmentation (arrow).
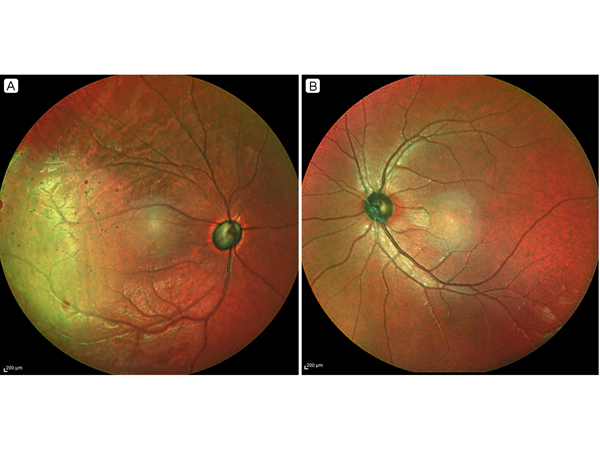
Figure 3.
Multicolor optical coherence tomography imaging. A, Right eye, showing advanced glaucomatous optic neuropathy. B, Left eye, showing a normal optic disc.
Multicolor optical coherence tomography imaging. A, Right eye, showing advanced glaucomatous optic neuropathy. B, Left eye, showing a normal optic disc.
Video 1.
Slit-lamp examination of the right eye revealed very prominent
iridonesis and phacodonesis, seen after each blink. This was also
observed in the left eye.
Slit-lamp examination of the right eye revealed very prominent
iridonesis and phacodonesis, seen after each blink. This was also
observed in the left eye.
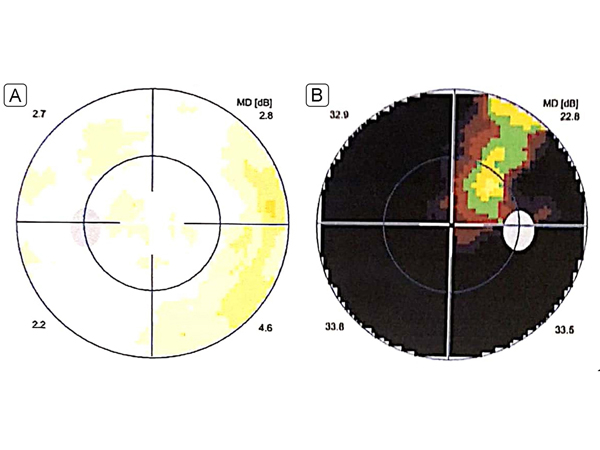
Figure 4.
Perimetry performed after definitive management (surgery and laser iridotomy). A, Left eye, showing a normal visual field. B, Right eye, showing a severely constricted field sparing a superotemporal island.
Perimetry performed after definitive management (surgery and laser iridotomy). A, Left eye, showing a normal visual field. B, Right eye, showing a severely constricted field sparing a superotemporal island.
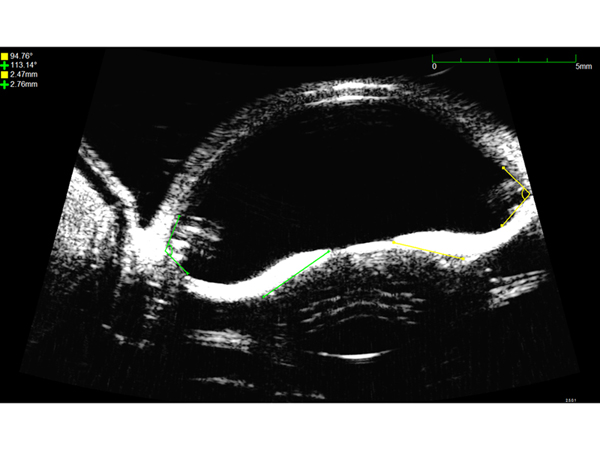
Figure 5.
Ultrasound biomicroscopy of the left eye showing peripheral posterior bowing (arrows) of the iris prior to laser peripheral iridotomy, with hypereflective zonules (asterisks).
Ultrasound biomicroscopy of the left eye showing peripheral posterior bowing (arrows) of the iris prior to laser peripheral iridotomy, with hypereflective zonules (asterisks).
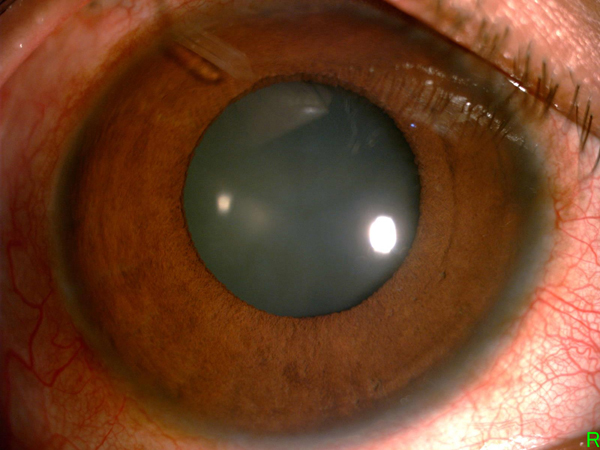
Figure 6.
Anterior segment photograph of the right eye 1 week after glaucoma drainage device insertion showing the tube visible superotemporally (arrow).
Anterior segment photograph of the right eye 1 week after glaucoma drainage device insertion showing the tube visible superotemporally (arrow).
Bilateral iridodonesis and phacodonesis in our patient was probably due to the zonular stretching caused by enlarged ciliary rings. The unilateral advanced glaucoma in the right eye (with unilateral hyper-pigmented PTM), without any of the other typical characteristics of pigment dispersion syndrome, was noteworthy, as was the lack of evidence of glaucoma in the contralateral eye, despite both eyes presenting with megalocornea, phacodonesis, and iridodonesis. We had difficulty making a definitive diagnosis of pigmentary glaucoma in the right eye, and we were uncertain whether the left eye would develop glaucoma. During initial presentation with high IOP, there were no signs of active pigment dispersion. We hypothesize that the glaucoma in the right eye was probably due to another secondary open-angle glaucoma etiology, such as an abundance of trabecular meshwork mesenchymal tissue or goniodysgenesis;(4) however, we could not entirely rule out a pigment dispersion component because of the hyperpigmented PTM in the right eye. Weak zonules could cause angle closure glaucoma by forward movement of the lens-iris diaphragm, but the angles were wide open in our case. Our patient has been doing well with the implant in the right eye, with IOP of 18 mm Hg without glaucoma medication. After more than 1 year, the vision in the right eye has deteriorated because of cataract development.
This case highlights the fact that patients with megalocornea should be monitored for glaucoma, especially those with other ocular findings. LPI was performed in the left eye, even though we were unsure whether this was a PDS case, because this was the patient’s good (glaucoma-free) eye, and the patient was very young. On UBM of the left eye, the reverse pupillary block seemed to have reversed after LPI.
2. Tsai CK, Lai IC, Kuo HK, Teng MC, Fang PC. Anterior megalophthalmos. Chang Gung Med J 2005; 28:191-5.
3. Meire FM, Delleman JW. Biometry in X linked megalocornea: pathognomonic findings. Br J Ophthalmol 1994;78:781-5.
4. Turaçlı ME, Tekeli O. Anterior megalophthalmos with pigmentary glaucoma. Graefe’s Graefes Arch Clin Exp Ophthalmol 2005;243:1066-8.